What is the role of antibody testing in myasthenia gravis?

have already shared their stories
TL;DR
- Antibody testing helps explain why muscle weakness occurs in myasthenia gravis (MG).
- The most common antibodies are AChR, MuSK, and LRP4.
- A negative antibody test does not rule out MG.
- Results are always interpreted together with symptoms and other examinations.
What is the role of antibody testing in myasthenia gravis?
Antibody testing helps doctors identify immune system markers that are commonly associated with myasthenia gravis and supports the overall understanding of the condition.
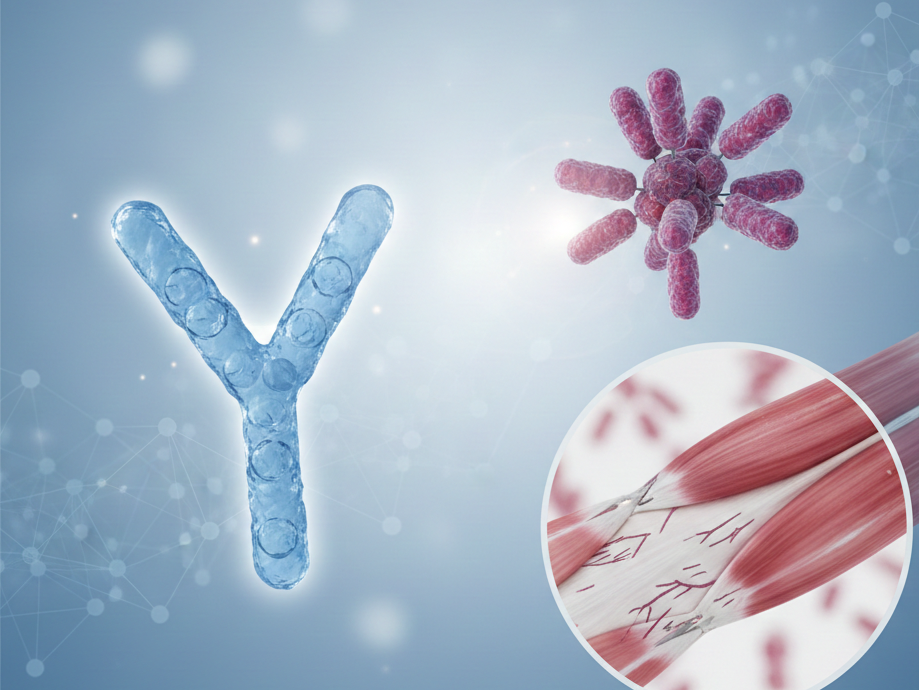
Myasthenia gravis is considered an autoimmune condition. In many people, the immune system produces antibodies that interfere with communication between nerves and muscles. Blood tests can sometimes detect these antibodies and provide clues about the underlying mechanism of muscle weakness.
Antibody testing does not work as a standalone answer. Instead, it is one piece of a broader diagnostic and clinical picture.
Why are antibodies important in myasthenia gravis?
In healthy muscle function, nerves release chemical signals that bind to receptors on muscle cells, triggering contraction. In MG, certain antibodies can disrupt this process.
These antibodies may:
- Block receptors on the muscle
- Damage structures involved in signal transmission
- Reduce the efficiency of nerve–muscle communication over time
Understanding which antibodies are present can help doctors classify MG subtypes and explain symptom patterns.
Which antibodies are most commonly tested in MG?
Acetylcholine receptor (AChR) antibodies
AChR antibodies are the most frequently detected antibodies in MG.
They are found in:
- Most people with generalized MG
- About half of people with purely ocular MG
These antibodies interfere directly with acetylcholine receptors on muscle cells, reducing muscle activation during repeated use.
MuSK antibodies
MuSK (muscle-specific kinase) antibodies are less common but clinically important.
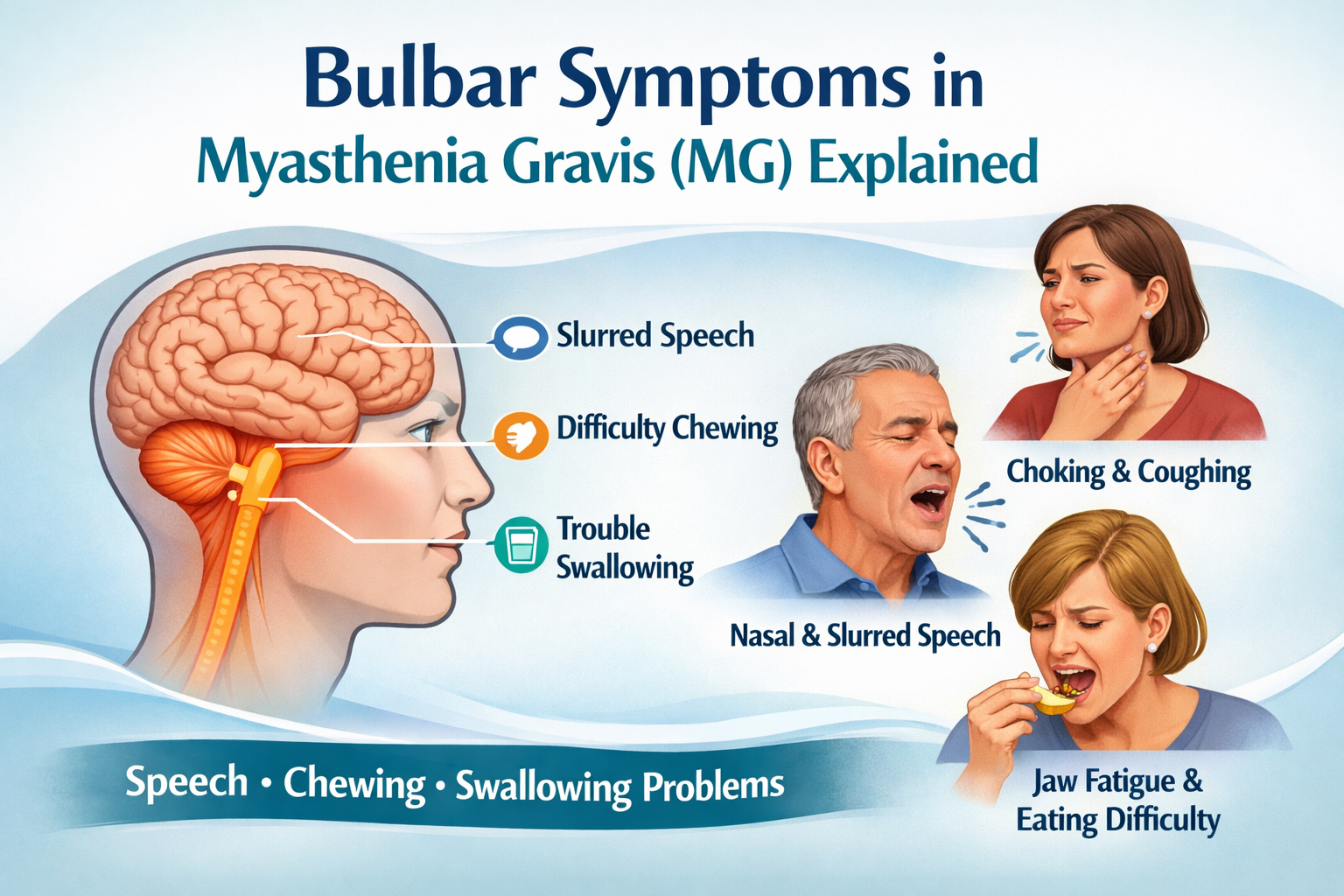
They are more often associated with:
- Prominent facial, throat, and neck weakness
- Speech and swallowing difficulties
- Different symptom distribution compared to AChR-positive MG
Not everyone with MG is tested for MuSK antibodies initially, but they are often considered when AChR tests are negative.
LRP4 antibodies
LRP4 antibodies are detected in a smaller group of people with MG.
They:
- Are not routinely tested in all healthcare settings
- May help explain symptoms in some antibody-negative cases
- Are still an area of ongoing research
What does a positive antibody test mean?
A positive antibody test supports the diagnosis of myasthenia gravis by showing immune activity commonly linked to the condition.
It can help:
- Confirm that symptoms are immune-mediated
- Distinguish MG from other neuromuscular conditions
- Guide further clinical evaluation
However, antibody levels do not reliably predict symptom severity or daily fluctuations.
Can antibody tests be negative in myasthenia gravis?
Yes. Some people have seronegative myasthenia gravis, meaning commonly tested antibodies are not detected in blood tests.
This can happen because:
- Current tests do not detect all possible antibodies
- Antibody levels may be very low
- Immune activity may involve mechanisms not captured by standard assays
A negative test result does not mean symptoms are “not real” or that MG is excluded.
How accurate are antibody tests?
Antibody tests are highly specific but not fully sensitive.
This means:
- A positive result is usually meaningful
- A negative result does not rule out MG
Sensitivity varies depending on:
- MG subtype (ocular vs generalized)
- Antibody type
- Stage of disease
Because of this, doctors rarely rely on antibody testing alone.
How are antibody test results interpreted together with other findings?
Antibody results are usually considered alongside:
- Symptom patterns and daily fluctuations
- Neurological examination
- Nerve and muscle studies
- Imaging of the chest (to assess the thymus)
This combined approach helps build a more accurate understanding of the condition over time.
—> Read this related article: Diagnosing Myasthenia Gravis: Key Tests and Procedures
Do antibody levels change over time?
Antibody levels can fluctuate, but changes do not always correlate with how a person feels day to day.
Some people:
- Have stable antibody levels with fluctuating symptoms
- Show antibody changes without noticeable symptom shifts
For this reason, antibody levels are generally not used to monitor daily disease activity.
What role does the thymus play in antibody production?
The thymus is involved in immune system development and may contribute to antibody production in MG.
In some people with MG:
- The thymus is enlarged
- A thymoma (thymus tumor) is present
- Immune regulation within the thymus is altered
This connection explains why thymus evaluation is often part of the broader MG assessment.
For more on the thymus read up here: Thymus and Myasthenia Gravis: Thymectomy, Thymoma, and Thymic Hyperplasia
What questions do patients often have about antibody testing?
People living with MG frequently wonder:
- Why results differ between individuals
- Whether antibody levels explain fatigue
- Why symptoms can worsen despite stable test results
These uncertainties are common and reflect the complexity of MG rather than test failure.
How can patients use antibody test results meaningfully?
While antibody tests do not provide all answers, they can help patients:
- Understand the autoimmune nature of MG
- Prepare informed questions for medical appointments
- Make sense of why symptoms fluctuate
Keeping a symptom history alongside test results can support clearer communication with healthcare professionals.
This content is informational and not a medical device.
mama health offers information and support and does not replace a doctor.

have already shared their stories
Sources
1. Gilhus NE. Myasthenia Gravis. New England Journal of Medicine. 2016.2. Gilhus NE et al. Myasthenia gravis. The Lancet Neurology. 2019.3. Sanders DB et al. International Consensus Guidance for Management of MG. Neurology. 2016.4. Myasthenia Gravis Foundation of America (MGFA). Antibody Testing Resources.5. European Academy of Neurology. MG Clinical Guidelines.