Understanding Antibodies in Myasthenia Gravis


have already shared their stories
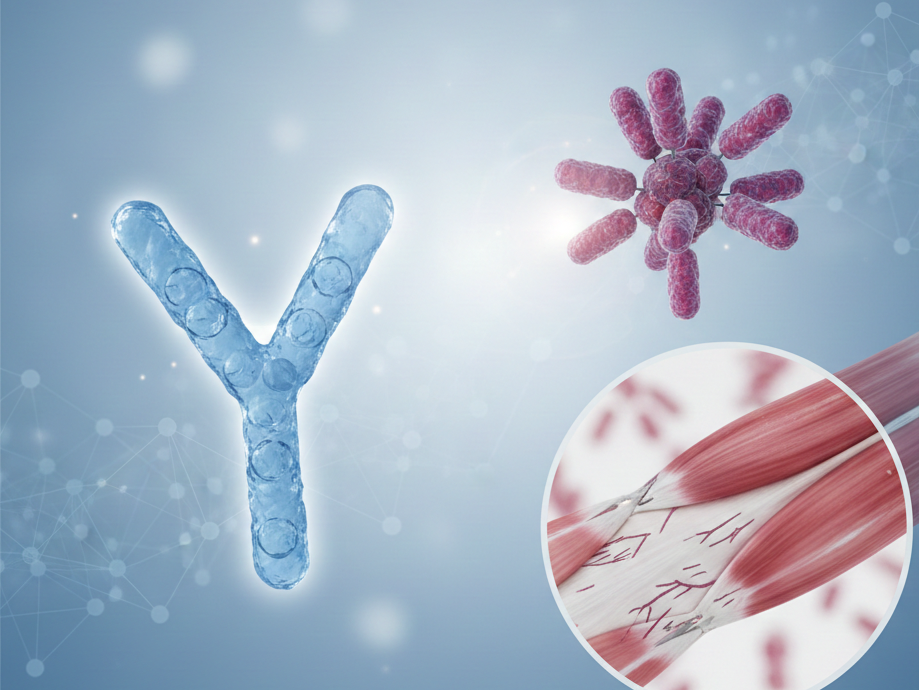
Myasthenia Gravis (MG) is a complex autoimmune disorder that affects neuromuscular transmission, leading to muscle weakness and fatigue. Central to understanding MG is the role that antibodies can play in many patients. This blog post will explore several antibody types associated with MG, emphasize their importance in diagnosis while clarifying their limitations, and discuss how they fit into a broader clinical context.

Anti-Acetylcholine Receptor Antibodies in Myasthenia Gravis
Anti-Acetylcholine receptor (AChR) antibodies are the most commonly detected antibodies in MG. These antibodies target the acetylcholine receptors at the neuromuscular junction, blocking or reducing the availability of acetylcholine, a neurotransmitter essential for muscle contraction. Patients with AChR antibodies typically experience muscle weakness and fatigue, which can worsen with activity.
Approximately 85 percent of Myasthenia Gravis patients have detectable AChR antibodies in their blood, making this a valuable biomarker in diagnosis. However, while a positive anti-AChR test strongly suggests MG, the diagnosis must always be supported by clinical symptoms and additional testing. Understanding the role of these antibodies helps guide treatment strategies, particularly therapies aimed at reducing their production or mitigating their effects. Nevertheless, treatment decisions are based on more than just antibody status, as symptom severity and response to medication vary widely among patients.
Anti-MuSK Antibodies and Myasthenia Gravis
Anti-MuSK antibodies are another subset of antibodies in MG. MuSK, or Muscle-Specific Kinase, is crucial for the formation and maintenance of the neuromuscular junction. These antibodies interfere with MuSK function, leading to severe disruptions in neuromuscular transmission.
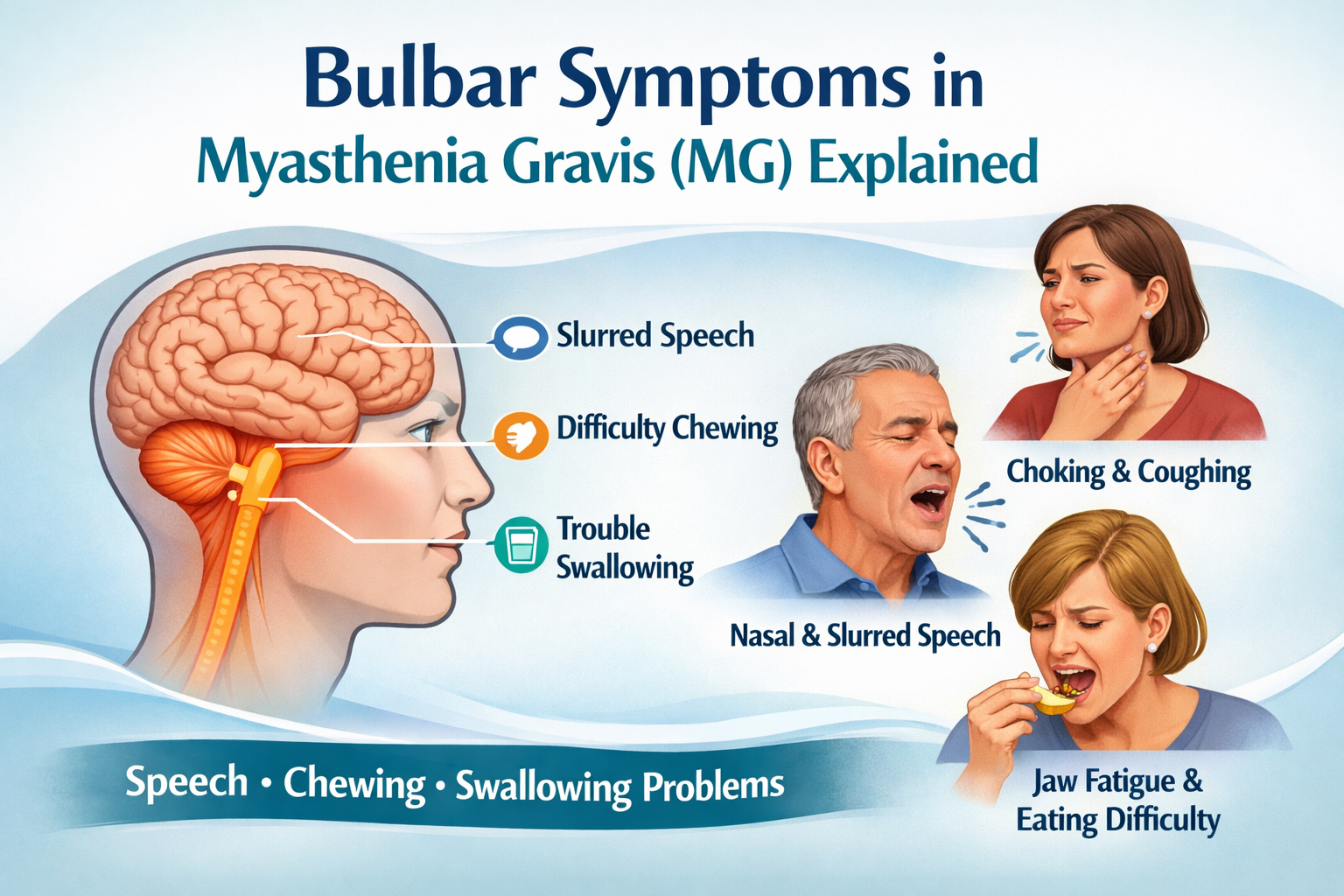
While less common than AChR antibodies, Anti-MuSK antibodies are present in about 10 to 15 percent of MG patients who test negative for AChR antibodies. Patients with Anti-MuSK antibodies often have more pronounced bulbar symptoms, such as difficulty speaking and swallowing, and may not respond as well to some of the standard MG treatments. Identifying the presence of these antibodies helps differentiate among MG subtypes and guides a more individualized treatment approach.
Anti-LRP4 Antibodies and Myasthenia Gravis
Anti-LRP4 antibodies represent another important group in MG. LRP4, or Low-Density Lipoprotein Receptor-Related Protein 4, plays a crucial role in neuromuscular junction function by interacting with MuSK.
These antibodies are found in a smaller subset of MG patients, particularly those who test negative for both AChR and MuSK antibodies. Anti-LRP4 antibodies interfere with the interaction between LRP4 and MuSK, further disrupting neuromuscular transmission and contributing to muscle weakness. Although less common, the detection of these antibodies provides valuable insight into MG’s diversity and helps refine diagnosis and treatment strategies.
Seronegative Myasthenia Gravis (SNMG)
A critical aspect of MG diagnosis is recognizing seronegative Myasthenia Gravis. While antibodies play an important role in many patients, up to 10 to 15 percent of MG patients have no detectable AChR, MuSK, or LRP4 antibodies, even with advanced testing methods. These individuals still exhibit classic MG signs and symptoms, and their diagnosis relies primarily on clinical evaluation rather than antibody tests.
The diagnosis of seronegative MG is based on clinical presentation, including muscle weakness patterns and fatigue, along with specialized electrophysiological tests such as repetitive nerve stimulation or single-fiber electromyography (EMG). Pharmacological tests, such as a pyridostigmine trial, can also be useful in supporting a diagnosis. Importantly, seronegative patients often respond to the same treatments as seropositive patients, reinforcing the need for a thorough clinical assessment rather than reliance on antibody testing alone.
Role of Antibodies in Myasthenia Gravis Diagnosis
Antibody testing is one component of MG diagnosis, but it is not the sole determinant. While detecting specific antibodies such as AChR, MuSK, or LRP4 can strongly support a diagnosis, clinical evaluation remains essential. Physicians must consider symptom presentation, response to medication, and electrophysiological test results to confirm the condition.
A negative antibody test does not exclude MG, nor does a positive test confirm it without clinical and electrophysiological correlation. Many MG patients, particularly those who are seronegative, rely on other diagnostic measures, such as repetitive nerve stimulation and single-fiber EMG, which detect impaired neuromuscular transmission even in the absence of antibodies. The pyridostigmine response test or the historically used edrophonium test can also provide diagnostic insights.

The management of MG is based on the patient’s overall clinical picture rather than antibody status alone. The severity of MG symptoms does not always correlate with antibody levels, as some patients with low antibody concentrations experience severe symptoms, while others with high levels may have milder disease.
Conclusion
Antibodies, such as Anti-Acetylcholine receptor, Anti-MuSK, and Anti-LRP4, play a significant role in many cases of Myasthenia Gravis. They serve as valuable biomarkers that can enhance diagnostic certainty and guide some aspects of treatment. However, a substantial minority of MG patients have no detectable antibodies, and their diagnosis relies on clinical symptoms and specialized testing.
A holistic approach to MG diagnosis considers clinical presentation, electrophysiological tests, and symptom response to treatment, rather than depending solely on antibody detection. Similarly, treatment strategies are guided by disease severity, individual patient response, and evolving clinical needs rather than antibody status alone.
As research advances, our understanding of MG continues to improve, leading to more refined diagnostic techniques and better treatment options. Ensuring that all patients, regardless of antibody status, receive timely and appropriate care remains a priority in managing this complex autoimmune disorder.

have already shared their stories
Sources
- Myasthenia Gravis: Epidemiology, Pathophysiology and Clinical Management
McGrogan, A., Sneddon, S., & de Vries, C.S. (2021). Journal of Clinical Medicine, 10(11), 2235. doi: 10.3390/jcm10112235.
Link - Autoimmune Pathology in Myasthenia Gravis Disease Subtypes
Fichtner, M.L., Jiang, R., Bourke, A., Nowak, R.J., & O’Connor, K.C. (2020). Frontiers in Immunology, 11, 776. doi: 10.3389/fimmu.2020.00776.
Link - Myasthenia gravis: the future is here
Kaminski, H.J., et al. (2020). The Journal of Clinical Investigation, 130(12), 6792-6804. doi: 10.1172/JCI179742.
Link - Myasthenia Gravis: Autoantibody Specificities and Their Role in MG Management
Lazaridis, K., & Tzartos, S.J. (2020). Cells, 9(11), 2399. doi: 10.3390/cells9112399.
Link - Autoantibody Specificities in Myasthenia Gravis; Implications for Improved Diagnostics and Therapeutics
Lazaridis, K., & Tzartos, S.J. (2020). Frontiers in Immunology, 11, 48. doi: 10.3389/fimmu.2020.00048.
Link - Serological diagnosis of myasthenia gravis and its clinical significance
Li, Y., et al. (2019). Annals of Translational Medicine, 7(14), 29798. doi: 10.21037/atm.2019.07.14.
Link - Myasthenia gravis
Verschuuren, J.J.G.M., et al. (2019). Nature Reviews Disease Primers, 5(1), 79-94. doi: 10.1038/s41572-019-0079-y.
Link