Myasthenia gravis medications: what are the most common treatments?


have already shared their stories
TL;DR
- Myasthenia gravis (MG) is usually managed with symptom-relieving medicines and immune-modulating therapies.
- Acetylcholinesterase inhibitors are typically the first-line medication to improve muscle strength.
- Immunosuppressive treatments, including corticosteroids and other agents, aim to reduce the immune attack on the neuromuscular junction.
- Biologic therapies are increasingly used for certain antibody-positive or refractory MG types.
- Treatment choices depend on MG subtype, severity, age, and individual risk factors, and are always guided by a neurologist.
What medications are commonly used to treat myasthenia gravis?
The most common medications for myasthenia gravis fall into three main groups: symptomatic treatments, immunosuppressive therapies, and targeted biologics.
Each group has a different role. Some improve muscle function directly, while others reduce the immune system activity that causes MG.
What is the first-line medication for myasthenia gravis?
Acetylcholinesterase inhibitors are usually the first-line treatment for MG.
Acetylcholinesterase inhibitors
These medications increase the availability of acetylcholine at the neuromuscular junction, helping muscles contract more effectively.
Most commonly used:
- Pyridostigmine (Mestinon®)
Key points:
- Often the first medication prescribed after diagnosis
- Helps improve symptoms such as drooping eyelids, muscle weakness, and fatigue
- Does not change the underlying autoimmune process
- Effects are temporary and dose-dependent
Common side effects:
- Abdominal cramps
- Diarrhea
- Increased salivation or sweating
Which immunosuppressive drugs are used in myasthenia gravis?
Immunosuppressive medications reduce the immune system’s attack on the neuromuscular junction.
Corticosteroids
Prednisone is the most commonly used corticosteroid in MG.
Why it’s used:
- Effective in improving muscle strength in many patients
- Often introduced when symptoms are not adequately controlled with pyridostigmine
Considerations:
- Improvement may take weeks
- Long-term use can cause side effects such as weight gain, osteoporosis, diabetes, and infections
- Dosing is carefully adjusted to balance benefit and risk
Steroid-sparing immunosuppressants
These drugs are often added to reduce the need for long-term high-dose steroids.
Common options include:
- Azathioprine
- Mycophenolate mofetil
- Cyclosporine
- Tacrolimus
Key points:
- Slower onset of action (months rather than weeks)
- Used for long-term disease control
- Require regular blood monitoring
What biologic therapies are used for myasthenia gravis?
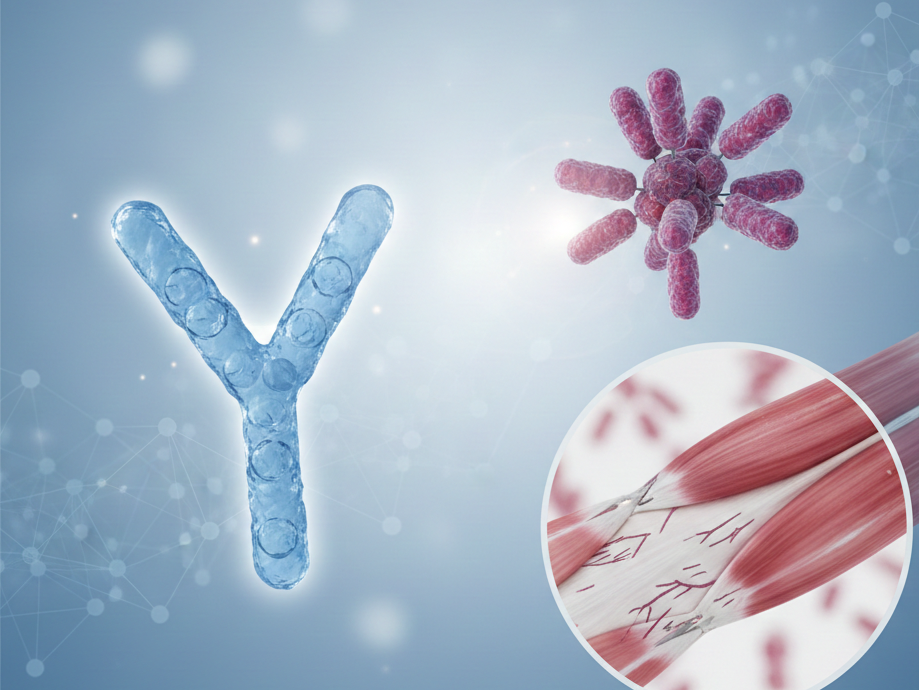
Biologic treatments target specific parts of the immune system involved in MG.
Complement inhibitors
Used mainly in anti-acetylcholine receptor (AChR) antibody–positive generalized MG.
Examples:
- Eculizumab
- Ravulizumab
Key points:
- Shown to reduce symptom severity in refractory MG
- Administered intravenously
- Increase susceptibility to certain infections, requiring vaccination
FcRn inhibitors
These therapies reduce circulating pathogenic antibodies.
Examples:
- Efgartigimod
- Rozanolixizumab
Key points:
- Approved for specific MG subtypes
- Can lead to faster symptom improvement in some patients
- Represent a newer class of MG treatments
When are short-term treatments like IVIG or plasma exchange used?
Intravenous immunoglobulin (IVIG) and plasma exchange are used for short-term symptom control.
IVIG
- Provides pooled antibodies that modulate immune activity
- Often used during disease exacerbations or before surgery
Plasma exchange (plasmapheresis)
- Removes circulating antibodies from the blood
- Used in myasthenic crisis or severe worsening
Important note:
These treatments are usually temporary measures and not long-term maintenance therapies.
Does everyone with myasthenia gravis use the same medications?
No, MG treatment is highly individualized.
Medication choices depend on:
- MG subtype (ocular vs. generalized)
- Antibody status (AChR, MuSK, LRP4)
- Symptom severity
- Age, pregnancy status, and other health conditions
Some people may manage symptoms with a single medication, while others require combination therapy.
How can people with myasthenia gravis stay informed about their treatment?
Living with MG often involves ongoing adjustments and discussions with healthcare providers. Many patients find it helpful to:
- Keep a medication and symptom timeline
- Note side effects or daily fluctuations
- Prepare questions before neurology visits
Educational tools and structured reflection can support more informed conversations with care teams.

have already shared their stories
Sources