Things to avoid with myasthenia gravis (MG)
.png)

have already shared their stories
TL;DR
- Some common medicines can worsen MG weakness, especially certain antibiotics, beta-blockers, magnesium (IV), and botulinum toxin.
- Heat, infections, stress, fatigue, and surgery are frequent triggers for worsening symptoms or crisis-like episodes.
- Don’t start, stop, or change prescriptions or supplements on your own—ask the prescriber to check MG safety first.
- Prepare a simple “MG safety checklist” for urgent care, dental work, imaging, and anesthesia so new clinicians don’t miss key risks.
What should you avoid if you have myasthenia gravis?
You should generally avoid known medication triggers and high-risk situations that can worsen muscle weakness, while adapting the details to your specific MG and medical history.
For most people, “things to avoid” falls into three buckets:
- Medications and procedures that can reduce neuromuscular transmission or stress breathing muscles,
- Everyday triggers like heat, illness/infection, sleep loss, and overexertion. Read about which foods to avoid here.
- Unplanned changes (new meds, missed doses, “quick” supplements) without an MG-aware check.
Which medications can make myasthenia gravis worse?
Some medications can worsen MG symptoms or trigger noticeable weakness, even if they are safe for many people without MG. Read this article on safe and unsafe medications for more detail.
Important nuance: a “cautionary drug” is not always “never use.” Many are used when benefits outweigh risks, but it helps to plan monitoring and alternatives.
High-signal “cautionary” categories (examples)
Below are commonly cited examples; brand names differ worldwide, so focus on generic names.
Certain antibiotics
Examples often flagged include fluoroquinolones (such as ciprofloxacin or levofloxacin), macrolides (such as azithromycin or erythromycin), and aminoglycosides (such as gentamicin).
These medications can interfere with neuromuscular transmission and may worsen muscle weakness in some people with myasthenia gravis.
If an antibiotic is needed, it can be helpful to ask whether an MG-safer alternative is available.
Heart and blood pressure medications
Beta-blockers are sometimes associated with increased weakness in people with myasthenia gravis.
When they are necessary, doctors often start with lower doses and monitor symptoms closely.
Minerals and supplements
Magnesium, especially when given intravenously, is considered potentially risky for people with myasthenia gravis.
Magnesium supplements or infusions should not be started casually and are best discussed with a healthcare professional who knows your MG history.
Neurology-related treatments
Botulinum toxin (Botox) is generally listed as a medication to avoid in myasthenia gravis because it can worsen neuromuscular weakness.
This includes both medical and cosmetic injections.
Other medications sometimes linked to symptom worsening
Some people report increased weakness with statins, procainamide, chloroquine or hydroxychloroquine, and iodinated contrast agents used in imaging.
These are not always contraindicated, but they usually require extra caution and symptom monitoring.
Which antibiotics are highest-risk in myasthenia gravis?
The antibiotics most consistently flagged are telithromycin, fluoroquinolones, macrolides, and aminoglycosides, because they have stronger evidence or warnings for MG worsening.
- Telithromycin is highlighted by MGFA as “should not be used in MG” (includes FDA black box warning context).
- Fluoroquinolones (e.g., ciprofloxacin, levofloxacin, moxifloxacin) are associated with worsening; MGFA advises caution “if at all.”
- Macrolides (e.g., azithromycin, erythromycin, clarithromycin) may worsen MG and are often treated as “use cautiously.”
- Aminoglycosides (e.g., gentamicin, tobramycin, neomycin) may worsen MG and are usually reserved when alternatives don’t fit.
If you need an antibiotic urgently, a helpful script is:
“I have myasthenia gravis. Can you check whether this antibiotic is cautionary in MG, and what alternatives exist?”
What supplements and over-the-counter products should you be careful with?
You should be careful with magnesium-containing products and “new” supplements because they can change neuromuscular signaling or interact with prescriptions in unpredictable ways.
Examples that commonly surprise people:
- Magnesium: MGFA specifically warns it can be “potentially dangerous” when given IV, and recommends close observation if used.
- Sleep aids and sedating cold/allergy medicines: not MG-specific “bans,” but sedation can complicate swallowing, breathing comfort, and fatigue—especially during infections or flare-like periods. (Discuss with a pharmacist/clinician who knows your meds.)
- “Muscle” or “recovery” supplements: formulas vary by country and may include magnesium, stimulants, or herbs that affect sleep and fatigue.
Practical rule: avoid starting any supplement without checking with your pharmacist or clinician and bringing your full medication list.
What lifestyle triggers can make myasthenia gravis symptoms worse?
Lifestyle and body-stress triggers can worsen MG because they increase fatigue or reduce your body’s “reserve,” making weakness show up sooner.
Commonly cited triggers include:
- Illness or infection
- Stress and fatigue
- Surgery
- Medication changes or reactions
- Heat exposure (many people report heat makes weakness more noticeable)
What “avoid” looks like in real life is often pacing:
- Avoid stacking high-energy tasks back-to-back.
- Avoid exercising through clear fatigue signals; build rest breaks in.
- Avoid skipping sleep when you notice your “weakness window” is getting earlier in the day.
How can heat and fever affect myasthenia gravis?
Heat can exacerbate MG symptoms in some people, often showing up as faster fatigue, heavier eyelids, or more generalized weakness.
Ways people commonly reduce heat impact:
- Avoid hot baths, hot tubs, and saunas during periods of unstable symptoms.
- Use cooling strategies (shade, hydration routines, cool packs) when temperatures climb.
- Treat fever as a “signal” to check in with a clinician—fever often means infection, which is a common MG stressor.
When should you seek urgent help for possible myasthenic crisis?
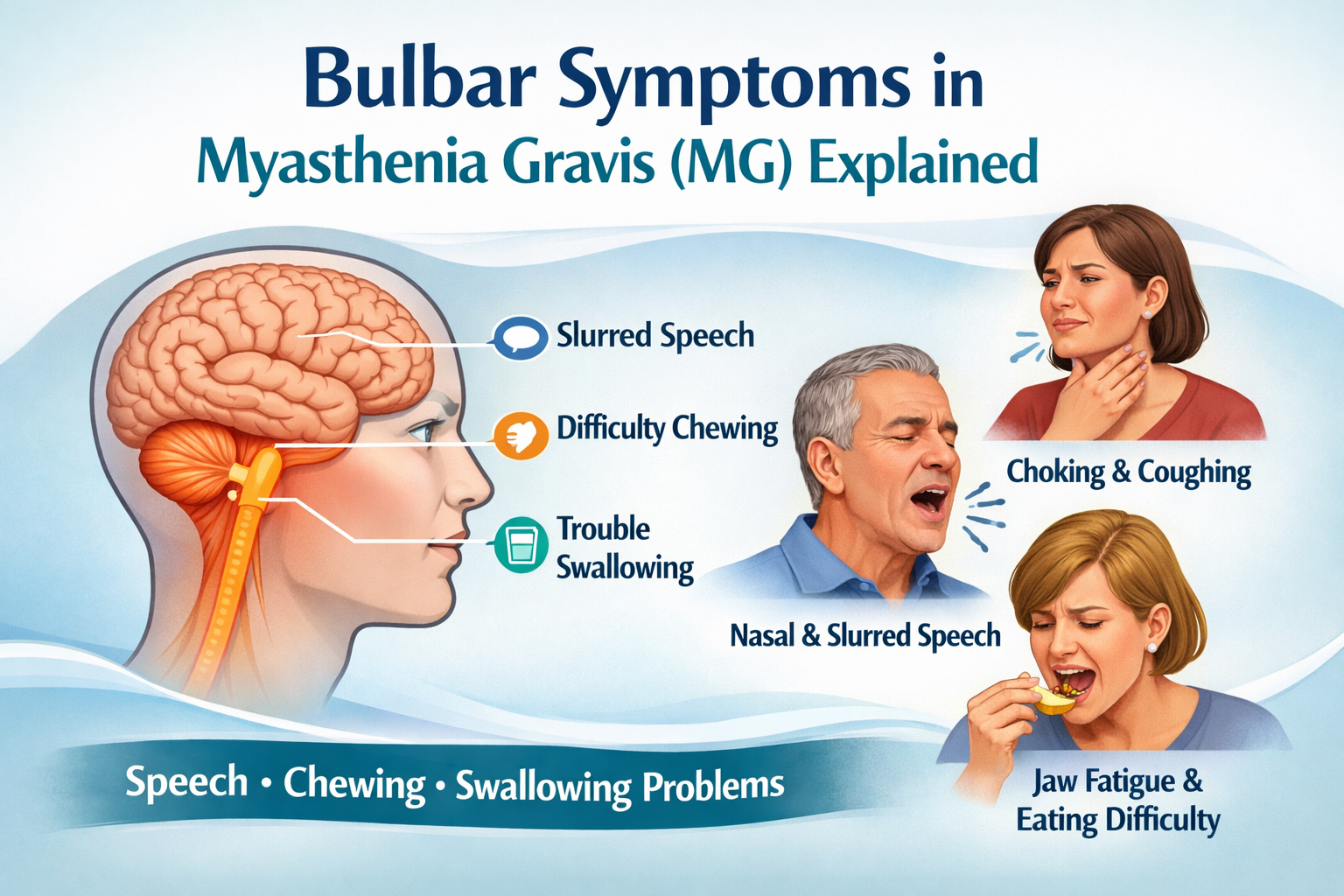
You should seek urgent help if you have new or rapidly worsening breathing, swallowing, or neck/face weakness, because myasthenic crisis involves respiratory and airway muscle weakness and can become life-threatening.
Red flags that warrant emergency assessment:
- Trouble breathing, counting, or speaking full sentences
- Choking, inability to swallow saliva, or repeated aspiration/coughing with sips
- Rapid progression of weakness (hours to a day), especially during infection or after a new medication
NINDS notes that myasthenic crisis can be triggered by infection, stress, surgery, or an adverse medication reaction, and estimates ~15–20% of people with MG experience crisis at some point.
How can you build a personal “avoid list” that actually works?
You can build a useful avoid list by combining (1) a medication safety check, (2) your known triggers, and (3) an emergency plan you can share quickly.
A simple 10-minute setup:
- Write your baseline symptoms (e.g., ptosis, double vision, chewing fatigue, limb weakness) and what “worse than usual” looks like.
- Keep one updated medication list (prescriptions, OTC, supplements) in your phone.
- Add an MG caution note: “Please check MG cautionary drugs before prescribing.”
- List your personal triggers (heat, poor sleep, infections, menstrual cycle, stress) and what helped last time.
- Prepare one sentence for urgent care: “I have MG; I’m worried about breathing/swallowing weakness; please assess for myasthenic crisis and review medications.”
mama health helps you record and reflect on symptoms and daily experiences, so you can bring a clearer summary and questions to your next visit.
Disclaimer:
Always consult with healthcare providers before starting or stopping any medication, and stay informed about the latest updates in MG treatment to ensure the best possible care. Regularly review resources on things to avoid and safe antibiotics to maintain optimal health management.
This content is informational and not a medical device.
mama health offers information and support and does not replace a doctor.

have already shared their stories
Sources
1. Myasthenia Gravis Foundation of America (MGFA). Cautionary Drugs (includes antibiotic and medication cautions).
2. Mayo Clinic. Myasthenia gravis – Symptoms and causes (factors that can make MG worse, examples of medicines).
3. NHS Scotland (Scottish Medicines). Myasthenia Gravis or Lambert-Eaton: Medicines that may affect patients (prescribing caution list).
4. Narayanaswami P, et al. International Consensus Guidance for Management of Myasthenia Gravis (update) (Neurology).
5. Johns Hopkins Medicine. Myasthenia Gravis (myasthenic crisis triggers and description).
6. NINDS (NIH). Myasthenia Gravis (crisis triggers; ~15–20% estimate).
7. Neuman A, et al. Anesthesia for Patients With Myasthenia Gravis (NCBI Bookshelf).
8. myaware (UK). Drugs to Avoid (patient-facing caution list, telithromycin emphasis).
9. MGFA. Beating the Heat During Summer Months (heat and symptom management tips).