Why do MG symptoms vary during the day?


have already shared their stories
TL;DR
- Myasthenia gravis (MG) causes fluctuating muscle weakness that often worsens with activity and improves with rest.
- Symptoms are usually milder in the morning and increase later in the day due to neuromuscular fatigue.
- Physical effort, stress, infections, heat, and sleep quality can all influence daily symptom patterns.
- Day-to-day variation is common and does not mean the condition is progressing.
- Understanding these patterns can help patients reflect on their day and prepare questions for their doctor.
Why do MG symptoms often change throughout the day?
MG symptoms change during the day because repeated muscle use reduces effective nerve-to-muscle signaling, leading to increasing weakness over time.
In MG, the immune system interferes with communication at the neuromuscular junction, the site where nerves activate muscles. With repeated use—such as talking, chewing, lifting objects, or walking—the signal becomes less efficient. Muscles that worked well earlier may weaken later, especially without rest.
Why are MG symptoms often better in the morning?
Symptoms are often better in the morning because muscles have rested overnight, allowing nerve-to-muscle signaling to temporarily recover.
During sleep, muscles are largely inactive. This rest helps replenish available signaling capacity at the neuromuscular junction. As a result, activities like opening the eyes, speaking, or walking may feel easier after waking than later in the day.
Why does muscle weakness worsen with activity in MG?
Muscle weakness worsens with activity because repeated use exhausts the already limited ability of nerves to activate muscles.
In MG, fewer functional receptors are available to respond to the nerve signal. Each muscle contraction uses part of this limited capacity. Over time, the signal weakens, and muscles respond less effectively. This is why symptoms such as drooping eyelids, slurred speech, or limb weakness can appear or intensify after sustained effort.
Do all muscles fluctuate in the same way?
No. MG affects different muscle groups differently, and fluctuations depend on how often a muscle is used.
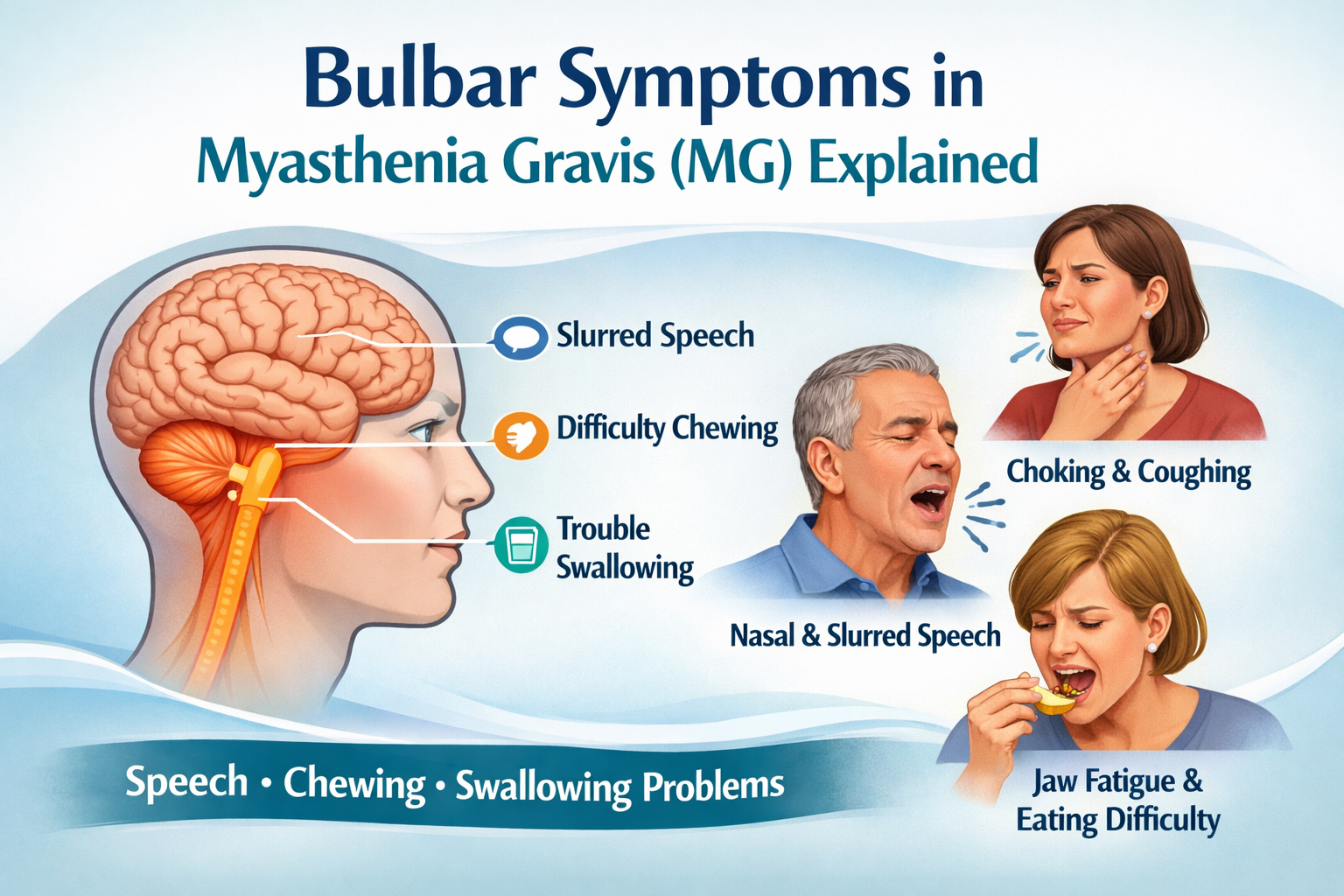
Commonly affected muscles include:
- Eye and eyelid muscles (double vision, drooping eyelids)
- Facial and throat muscles (speech and swallowing changes)
- Neck, arm, and leg muscles (head drop, difficulty lifting or walking)
Muscles used repeatedly during the day—like those involved in speaking or holding posture—often show earlier or more noticeable fatigue.
Can external factors make daily MG fluctuations worse?
Yes. Several external and lifestyle factors can intensify daily symptom variation.
These include:
- Physical or emotional stress
- Poor sleep or sleep deprivation
- Infections or fever
- Heat or high temperatures
- Extended periods without rest
These factors increase overall fatigue or place additional demands on muscles, making fluctuations more pronounced.
Is symptom variation a sign that MG is getting worse?
Not necessarily. Daily symptom variation is a core feature of MG and can occur even when the condition is otherwise stable.
Fluctuations alone do not indicate disease progression. Many people with MG experience predictable patterns—such as feeling stronger in the morning and weaker in the evening—over long periods of time.
Keeping track of when symptoms change during the day can help patients reflect on patterns and discuss them more clearly with their healthcare provider.
How can understanding daily patterns help people living with MG?
Understanding daily symptom patterns can help people plan activities, conserve energy, and communicate more effectively with their care team.
Examples include:
- Scheduling demanding tasks earlier in the day
- Allowing regular rest periods
- Noting triggers that worsen fatigue
- Preparing clear observations for medical appointments
This awareness supports informed conversations with clinicians without replacing professional medical advice.
Disclaimer:
This content is informational and not a medical device.
mama health offers information and support and does not replace a doctor.

have already shared their stories
Sources
1. Gilhus NE. Myasthenia Gravis. New England Journal of Medicine.
2. National Institute of Neurological Disorders and Stroke (NINDS). Myasthenia Gravis Fact Sheet.
3. Sanders DB et al. Clinical aspects of myasthenia gravis. Neurologic Clinics.
4. NHS UK. Myasthenia gravis overview.





.png)
.png)