Your personal
AI assistant for
Decompensated Cirrhosis
.avif)
.avif)
.avif)
.avif)
.avif)



.avif)

.avif)
.avif)
.avif)
.avif)



.avif)

.avif)
.avif)
.avif)
.avif)



.avif)

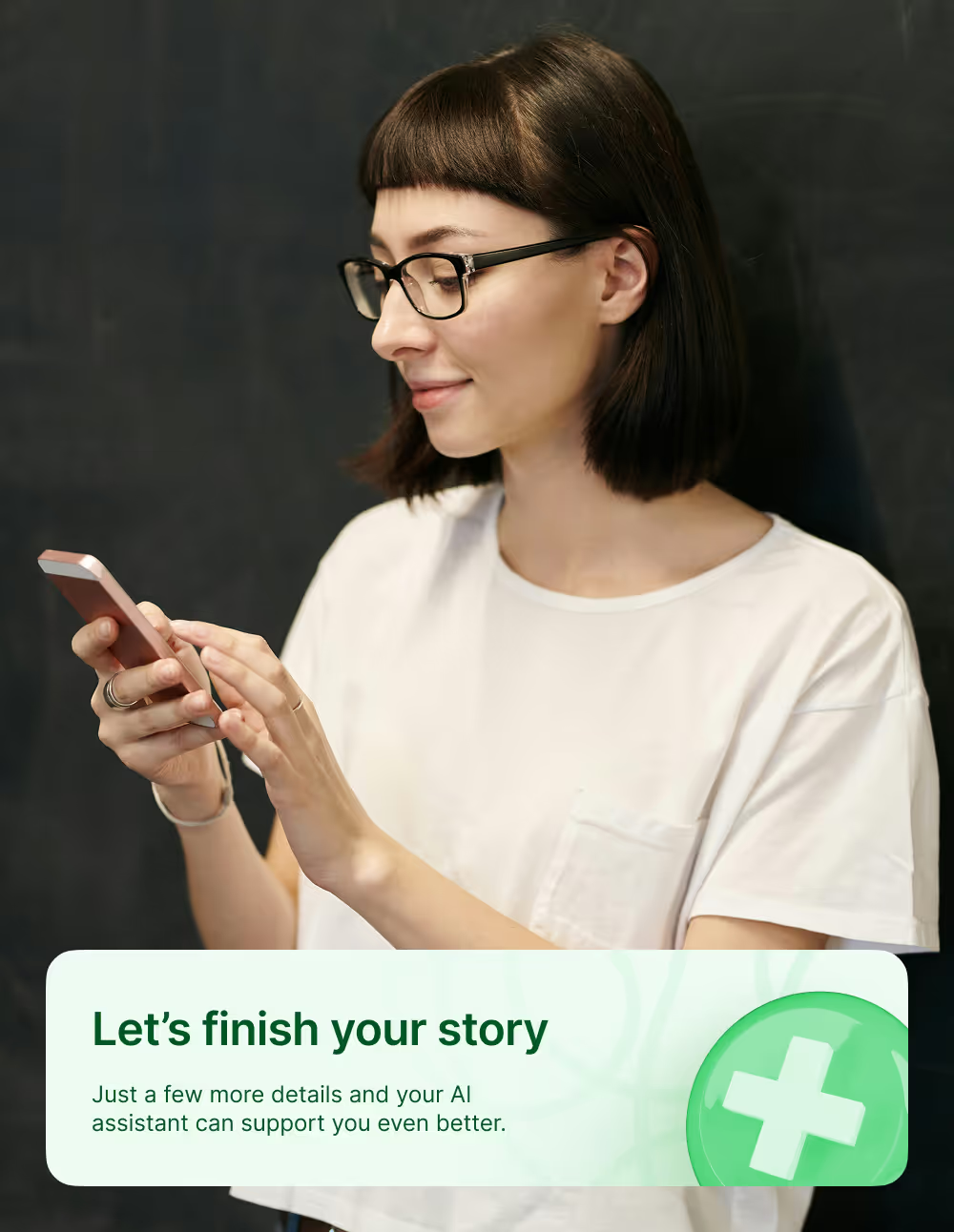
Our platform gives you a space to note your experiences, prepare for medical visits, and connect with insights shared by others affected by decompensated cirrhosis. Whether you’re trying to understand symptoms, adjust to new routines, or find the right questions to ask your doctor, mama health helps you stay organized and feel more informed.
You’re not alone in this — mama health is built to walk with you through the ups and downs of decompensated cirrhosis, helping you reflect on what matters most and advocate for your care.
What is Decompensated Cirrhosis?
Decompensated cirrhosis is an advanced stage of chronic liver disease in which the liver can no longer perform its essential functions well enough to keep the body stable. Many people live for years with compensated cirrhosis, meaning the liver is heavily scarred but still manages to work sufficiently, often with few or no symptoms.
Decompensation occurs when the liver’s function declines to the point where serious complications appear. These complications signal that the body can no longer compensate for liver damage.


The shift from compensated to decompensated cirrhosis can be gradual or sudden. It is often triggered by factors such as infections, alcohol use, gastrointestinal bleeding, certain medications, dehydration, or the natural progression of liver scarring. Once decompensation occurs, patients typically experience one or more of four major complications:
1. Ascites
Ascites is the abnormal buildup of fluid in the abdomen and is the most common sign that cirrhosis has decompensated.
Why it happens:
As liver function declines, pressure increases in the portal vein (portal hypertension). At the same time, the liver produces fewer proteins like albumin, which normally help keep fluid in the bloodstream. This combination causes fluid to leak into the abdominal cavity.
Possible symptoms:
- Increasing abdominal size or bloating
- Shortness of breath due to pressure on the diaphragm
- Early fullness when eating
- Weight gain from fluid, not fat
Ascites can range from mild to severe, and complications like spontaneous bacterial peritonitis (SBP) can develop, which is a medical emergency.
2. Variceal Bleeding
Variceal bleeding occurs when swollen veins in the esophagus or stomach—called varices—burst due to high pressure in the portal vein.
Why it happens:
Portal hypertension forces blood into smaller veins that were never meant to handle such pressure. Over time, these veins enlarge and become fragile.
Why it signals decompensation:
Once varices bleed, the risk of future bleeding increases, and the overall risk of mortality rises.
Possible symptoms:
- Vomiting blood
- Black or tarry stools
- Lightheadedness or fainting
- Sudden weakness
Variceal bleeding is a medical emergency and requires immediate treatment.
3. Jaundice (Icterus)
Jaundice is yellowing of the skin and eyes due to a buildup of bilirubin, a pigment the liver normally processes and removes.
Why it develops:
As the liver becomes more damaged, it cannot properly clear bilirubin. Levels rise in the bloodstream, causing visible yellowing and sometimes itching.
Possible symptoms:
- Yellow eyes or skin
- Dark urine
- Pale stools
- Intense itching
- Fatigue
Jaundice is an important sign that liver function is deteriorating.
4. Hepatic Encephalopathy (HE)
Hepatic encephalopathy is a serious neurological complication and a major marker of decompensated cirrhosis. It occurs when toxins—especially ammonia—that the liver usually filters out begin to accumulate in the blood and reach the brain.
Why HE Happens in Decompensated Cirrhosis
When the liver can no longer detoxify substances or regulate metabolic processes effectively, toxins build up. At the same time, changes in gut bacteria, inflammation, and altered neurotransmission further disrupt brain function.
Triggers such as infections, constipation, dehydration, gastrointestinal bleeding, or certain medications can rapidly worsen HE.
How HE Affects the Brain
HE interferes with attention, memory, coordination, and behavior. Symptoms can range from subtle to life-threatening, and they often fluctuate over time, especially during acute episodes.
Common Symptoms of HE
- Mild confusion or “brain fog”
- Trouble concentrating or slowed thinking
- Mood changes or irritability
- Sleep disturbances (like reversed day–night cycles)
- Difficulty performing routine tasks
- Tremors or poor coordination
- Asterixis (flapping tremor of the hands)
- In advanced stages, disorientation, extreme drowsiness, or reduced consciousness
Why HE Is So Significant
HE often indicates that the liver is struggling to perform essential functions.
Frequent or severe episodes may mean that the disease is progressing, and they can significantly affect quality of life, independence, and safety.
How can mama health help?

Developed and supervised by medical experts
What patients are saying
There are so many testimonies and so many people like me.
I hope this platform grows so we can help so many people who feel alone with a disease.
In the end we are many and all together we can fight.❤️"
There are so many testimonies and so many people like me.
I hope this platform grows so we can help so many people who feel alone with a disease.
In the end we are many and all together we can fight.❤️"
Frequently asked questions
The healthcare system is missing a crucial piece—real patient experiences. We bring those voices back into the system, making healthcare truly patient-centric. By connecting data from patients, doctors, hospitals, and research, we help unlock new insights, improve treatments, and turn today’s incurable diseases into tomorrow’s breakthroughs.
- See what works – Learn from others with the same condition and avoid trial-and-error treatments.
- Get a clear health picture – Track your journey, compare with others, and gain deeper understanding.
- Be part of something bigger – Your experience helps improve healthcare and accelerate research.
We use the information shared on mama health to improve treatments and services for all patients. However, we ensure that no one—neither other patients, scientists, nor healthcare companies—can identify you personally.
To request the deletion of your data, simply send an email to support@mamahealth.com.

.avif)

.avif)