Pregnancy and myasthenia gravis: what is known? (January 2026)

have already shared their stories
TL;DR
- Pregnancy is often possible and safe for people with myasthenia gravis (MG), but requires planning and close medical follow-up.
- MG symptoms may improve, worsen, or stay stable during pregnancy; changes are unpredictable.
- Certain MG medications are considered compatible, while others should be avoided during pregnancy and breastfeeding.
- Newborns can rarely develop transient neonatal myasthenia, which usually resolves within weeks.
Why does pregnancy require consideration for patients with MG?
Myasthenia gravis is a chronic autoimmune neuromuscular condition that causes fluctuating muscle weakness.
Pregnancy matters because hormonal and immune changes can influence disease activity, and some MG treatments may affect the developing fetus.
Most people with MG can become pregnant and deliver safely, but outcomes are best when pregnancy is planned during a stable phase of disease and managed by a multidisciplinary care team.
Is pregnancy safe if you have MG?
Yes, pregnancy is generally safe for people with MG, but it is still considered high-risk and thus requires specialist monitoring.
Large observational studies show that:
- Fertility is usually normal in people with MG,
- Rates of miscarriage and congenital malformations are similar to the general population,
- Maternal complications are more likely if MG is poorly controlled before conception.
Stability of symptoms before pregnancy is one of the strongest predictors of a smoother course.
How can MG symptoms change during pregnancy?
MG symptoms can change at any time during pregnancy, but patterns are variable.
Research suggests:
- About one-third of patients experience symptom worsening,
- About one-third remain stable,
- About one-third improve, often during the second trimester.
Symptom worsening is more common:
- In the first trimester,
- In the postpartum period, especially within the first 6 weeks after delivery.
Since changes are unpredictable, regular neurological follow-up is essential.
Which MG treatments are considered safer in pregnancy?
Some MG medications have longer safety experience in pregnancy, while others are avoided due to known risks.
Commonly used with caution (case-by-case):
- Pyridostigmine,
- Corticosteroids (e.g. prednisone).
Often avoided or discouraged:
- Mycophenolate mofetil (MMF),
- Methotrexate (MTX),
- Cyclophosphamide.
Treatment decisions are individualized and based on disease severity, prior response, and pregnancy stage. Medication changes should ideally happen before conception, not during pregnancy.
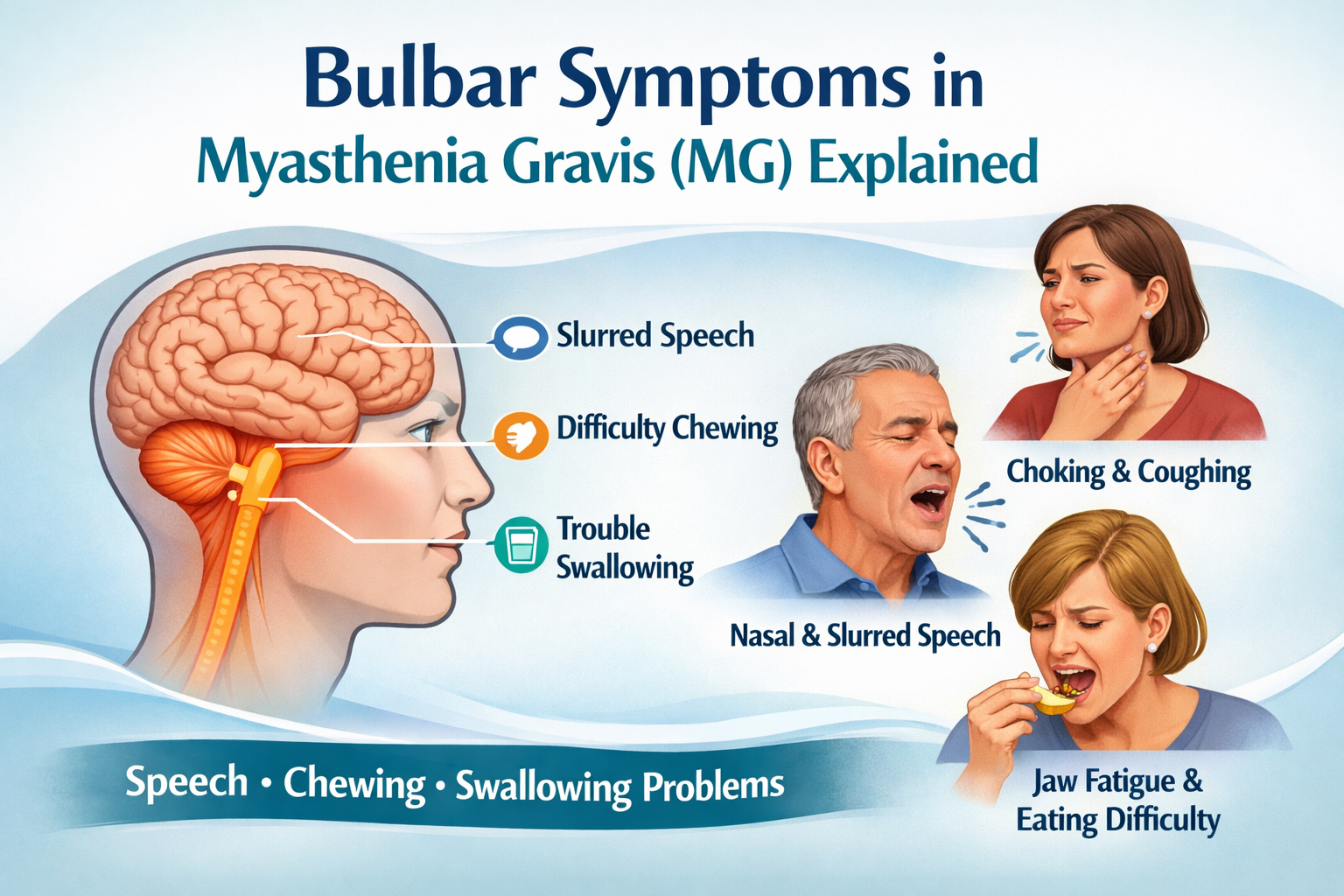
Can MG affect labor and delivery?
Most people with MG can have a vaginal delivery.
Important considerations include:
- Fatigue of respiratory and bulbar muscles during prolonged labor,
- Avoidance of medications that may worsen neuromuscular transmission,
- Planning anesthesia carefully, as some muscle relaxants can exacerbate weakness.
Cesarean section is usually reserved for obstetric reasons, not MG alone.
What is neonatal myasthenia and how common is it?
Transient neonatal myasthenia occurs when maternal antibodies cross the placenta and temporarily affect the baby.
Key points:
- Occurs in about 10–20% of newborns of mothers with MG,
- Symptoms may include weak cry, poor feeding, or low muscle tone,
- Symptoms usually appear within the first days of life,
- The condition is temporary and typically resolves within weeks as maternal antibodies disappear.
Neonatal myasthenia is not inherited and does not mean the child will develop MG later in life. For more detailed information read our article: Neonatal Myasthenia: Symptoms, Causes & Treatment.
Is breastfeeding possible with MG?
Breastfeeding is often possible for people with myasthenia gravis, depending on maternal strength, fatigue, and the medications used.
Pyridostigmine, corticosteroids (prednisone/prednisolone), azathioprine, intravenous immunoglobulin, and plasma exchange are generally considered compatible with breastfeeding, as only low amounts pass into breast milk and are not regarded as clinically significant for the infant.
In contrast, mycophenolate mofetil, methotrexate, and cyclophosphamide should be avoided during breastfeeding. Monoclonal antibodies (such as rituximab, eculizumab, and efgartigimod) and calcineurin inhibitors (cyclosporine, tacrolimus) require individualized risk–benefit assessment and close monitoring due to limited or variable safety data.
In either case any medication decision during breastfeeding should be discussed with neurology and obstetric teams to balance maternal health and infant safety.
What should be planned before pregnancy?
Preconception counseling is strongly recommended.
Topics usually include:
- Reviewing MG stability and recent exacerbations
- Adjusting medications to pregnancy-compatible options
- Planning delivery and postpartum support
- Discussing neonatal monitoring after birth
Early planning helps reduce avoidable risks for both parent and baby.
Disclaimer:
This content is informational and not a medical device.
mama health offers information and support and does not replace a doctor.

have already shared their stories
Sources
1. European Academy of Neurology. Management of myasthenia gravis guidelines.
2. American Academy of Neurology. Myasthenia gravis and pregnancy overview.
3. Gilhus NE et al. Myasthenia gravis and pregnancy. Neurology.
4. Sanders DB et al. International consensus guidance for management of myasthenia gravis.
5. NIH Genetic and Rare Diseases Information Center (GARD): Myasthenia gravis.
6. Gilhus NE Treatment Considerations in Myasthenia Gravis for the Pregnant Patient. Expert Review of Neurotherapeutics.





.png)
.png)