Why can the MG diagnosis take time?
.png)

have already shared their stories
TL;DR
- Myasthenia gravis (MG) often starts with fluctuating, non-specific symptoms.
- Early signs can mimic stress, eye problems, or other neurological conditions.
- Antibody tests and nerve studies are not always positive at first.
- Symptoms can improve temporarily, which may delay further investigation.
- Many people see multiple doctors before MG is confirmed.
What makes myasthenia gravis hard to recognize early?
MG is difficult to recognize because symptoms are variable, subtle, and fluctuate over time.
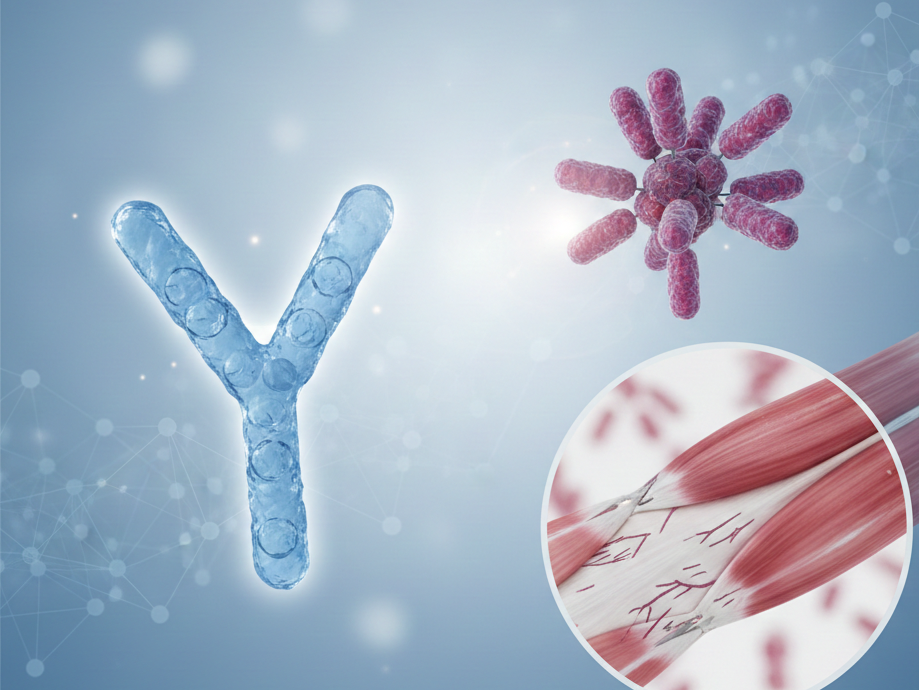
myasthenia gravis is a rare autoimmune condition that affects communication between nerves and muscles. Early symptoms may appear only after exertion and improve with rest, which can make them seem temporary or harmless.
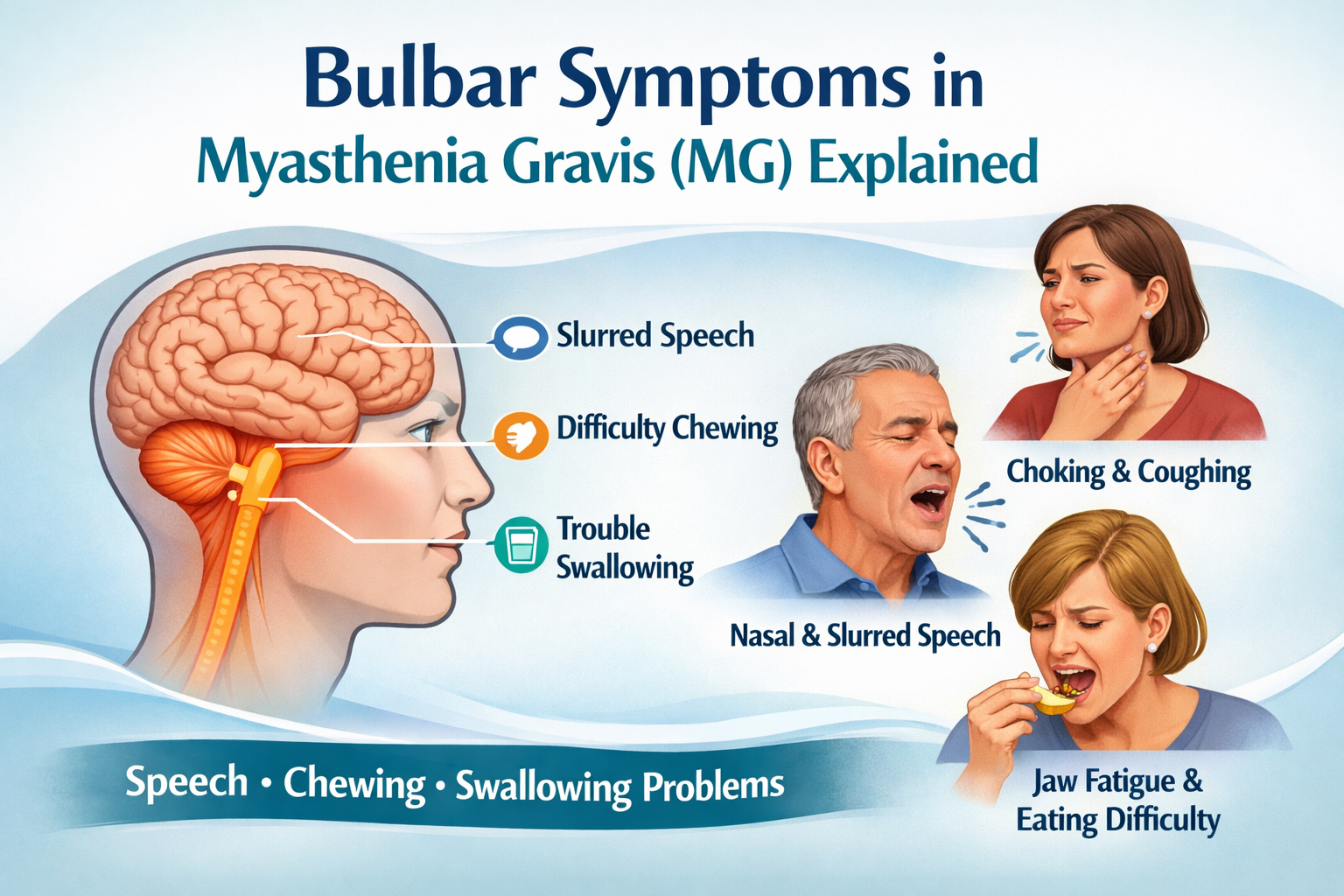
Common early signs include:
- Drooping eyelids (ptosis)
- Double vision
- Slurred speech late in the day
- Fatigue when chewing, speaking, or using arms
Because these symptoms come and go, they are often attributed to fatigue, stress, or aging.
Why do MG symptoms often get mistaken for other conditions?
MG symptoms overlap with many more common conditions, leading to misinterpretation.
Doctors may initially consider:
- Eye strain or ophthalmologic disorders (for double vision)
- Stroke or transient ischemic attack
- Multiple sclerosis
- Anxiety or functional neurological disorders
- General fatigue or burnout
Ocular MG, which affects only the eyes, is especially challenging because it can remain localized for months or years before other muscles are involved.
How do fluctuating symptoms delay diagnosis?
MG symptoms typically worsen with activity and improve with rest, which is unusual for many neurological diseases.
This fluctuation means:
- Symptoms may not be visible during a short clinic visit
- Neurological exams can appear normal earlier in the day
- Patients may struggle to describe symptoms clearly
As a result, clinicians may adopt a “wait and see” approach before ordering further tests.
Why aren’t tests always conclusive at first?
There is no single test that definitively diagnoses MG in every person.
Diagnostic tools include:
- Blood tests for acetylcholine receptor (AChR) or MuSK antibodies
- Repetitive nerve stimulation or single-fiber EMG
- Imaging of the thymus (CT or MRI)
However:
- Up to 10–15% of people with MG are seronegative, meaning standard antibody tests are negative
- Early disease may not yet show clear changes on nerve testing
- Access to specialized neuromuscular testing can take time
This often leads to repeated testing over months or years.
Does symptom improvement slow down diagnosis?
Yes. Temporary improvement can delay further investigation.
Some people notice that:
- Symptoms improve spontaneously
- Symptoms lessen during periods of rest or reduced stress
- Eye symptoms resolve and then return later
These changes can give both patients and clinicians the impression that the issue has resolved, postponing referral to a neurologist.
Why do many people see multiple doctors before diagnosis?
Because MG is rare and presents variably, diagnosis often requires specialist involvement.
Many patients report seeing:
- General practitioners
- Ophthalmologists
- ENT specialists
- Emergency physicians
- Multiple neurologists
Studies show that diagnostic delays of 1–3 years are not uncommon, particularly in ocular or mild generalized MG.
What usually leads to the final diagnosis?
Diagnosis is often made when:
- Symptoms become more persistent or generalized
- Weakness spreads beyond the eyes
- A neurologist familiar with neuromuscular disorders evaluates the case
- Repeat testing eventually becomes positive
Keeping a detailed symptom history can support this process by showing patterns that are otherwise easy to miss.
How can patients support the diagnostic journey?
While diagnosis must always be made by a clinician, patients can support the process by:
- Noting when symptoms worsen or improve
- Recording triggers such as fatigue, infections, or stress
- Tracking daily fluctuations
- Preparing clear descriptions for appointments
Tools, like mama health, that help patients reflect on symptom patterns over time can make conversations with healthcare professionals more precise and productive.
Disclaimer
This content is informational and not a medical device.
mama health offers information and support and does not replace a doctor.

have already shared their stories
Sources
1. Gilhus NE. Myasthenia gravis. N Engl J Med. 2016.
2. Sanders DB et al. International Consensus Guidance for Management of Myasthenia Gravis. Neurology. 2016.
3. National Institute of Neurological Disorders and Stroke (NINDS): Myasthenia Gravis Information Page.
4. Drachman DB. Myasthenia gravis. Semin Neurol. 2016.