Thymus and Myasthenia Gravis: Thymectomy, Thymoma, and Thymic Hyperplasia


have already shared their stories
The thymus gland plays a significant role in the development and management of Myasthenia Gravis (MG), an autoimmune disease affecting the neuromuscular junction. Understanding its function and the impact of thymus disorders is crucial for both patients and healthcare providers. In this blog post, we will explore the relationship between the myasthenia gravis thymus, focusing on thymectomy for myasthenia gravis, thymoma and Myasthenia Gravis, and the consequences of thymus gland removal for myasthenia gravis.
The Role of the Thymus in Myasthenia Gravis
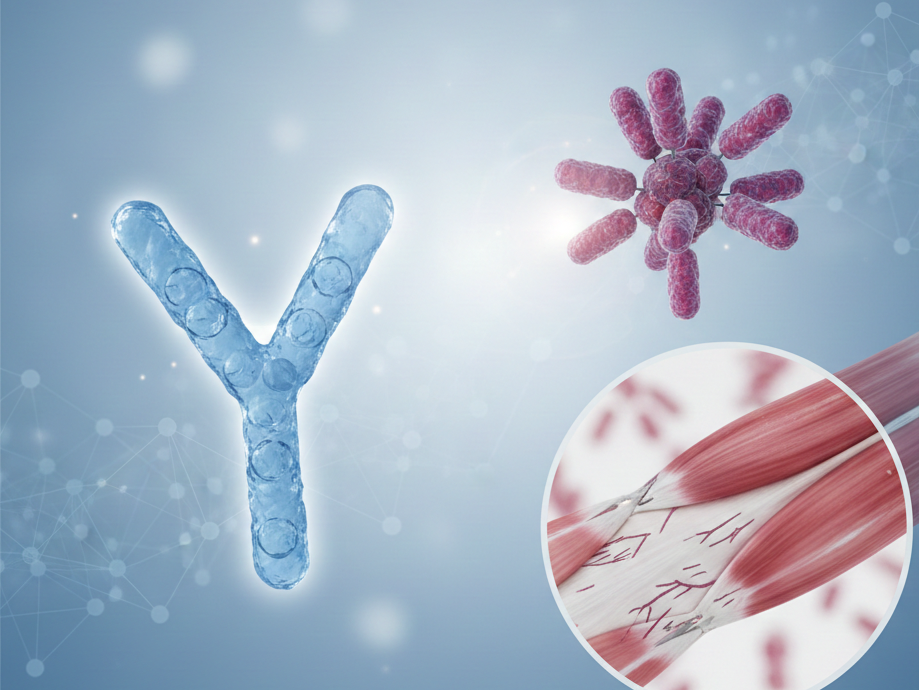
The thymus is a small gland located in the mediastinum, just behind the breastbone. It is essential for the development of the immune system, particularly in T-cell differentiation and the production of T-cells, which are crucial for immune response. The thymus contains thymic epithelial cells that play a vital role in this process. In Myasthenia Gravis, the thymus is often abnormal, and it is believed to play a role in the autoimmune response that targets acetylcholine receptors at the neuromuscular junction, leading to muscle weakness. This autoimmune attack involves anti-AChR antibodies (acetylcholine receptor antibodies), and in some cases, anti-MuSK antibodies.

Thymectomy in Myasthenia Gravis
What is Thymectomy?
Thymectomy, also known as thymus gland removal or thymus surgery, is the surgical removal of the thymus gland. But what is a thymectomy exactly? It is considered a treatment option for certain patients with Myasthenia Gravis, particularly those with thymoma (a tumor of the thymus) or thymic hyperplasia (enlargement of the thymus). The goal of thymectomy surgery is to reduce the abnormal immune response contributing to MG symptoms and potentially achieve remission. Thymectomy is a crucial form of myasthenia gravis surgery that can significantly impact the course of the disease.
Benefits of Thymectomy
Several studies, including the MGTX randomised trial, have shown that thymectomy can improve symptoms and reduce the need for immunosuppressive treatment in patients with Myasthenia Gravis. By removing the thymus, the autoimmune attack on neuromuscular junctions may be lessened, leading to better muscle function and overall symptom control. Thymectomy is most effective in patients with generalized Myasthenia Gravis and is often recommended for younger patients and those in the early stages of the disease. Many patients wonder, "Does thymectomy cure Myasthenia Gravis?" While it may not provide a complete cure, the benefits of thymectomy in Myasthenia Gravis can be significant, with improved remission rates and reduced reliance on medications like prednisone, corticosteroids, and pyridostigmine.
Surgical Approaches to Thymectomy
There are different surgical approaches to thymectomy, including traditional open surgery (transsternal approach) and minimally invasive techniques such as video-assisted thoracoscopic surgery (VATS) or thoracoscopic thymectomy. Extended thymectomy, which involves removing all thymic tissue and surrounding fat, is often preferred for optimal results. Minimally invasive thymectomy, including robotic-assisted thymectomy, often results in shorter recovery times and less postoperative discomfort. The choice of thymectomy procedure depends on factors such as the patient’s condition, the presence of thymoma, and the surgeon’s expertise. It’s worth noting that patients may have concerns about the thymectomy scar, which can vary depending on the surgical approach used. It is essential to note that, anesthesia in patients with myasthenia gravis requires special attention, as they are at increased risk for respiratory muscle weakness during and after surgery. Careful perioperative planning, including preoperative optimization and close postoperative monitoring, is essential to reduce the risk of complications such as respiratory failure.
Thymoma and Myasthenia Gravis
Understanding Thymoma
Thymoma is a tumor originating from the thymic epithelial cells of the thymus. It is relatively rare but has a significant association with Myasthenia Gravis, as approximately 10-15% of MG patients have a thymoma. Thymomas can be benign or malignant and may cause symptoms by compressing surrounding structures (compressive symptoms) or through their association with MG. In some cases, thymoma can lead to a mediastinal abnormality, which may be detected during diagnostic imaging.
Impact of Thymoma on Myasthenia Gravis
Patients with thymoma myasthenia gravis often experience more severe MG symptoms and may be at higher risk of myasthenic crisis. The presence of thymoma can complicate the management of Myasthenia Gravis, making timely diagnosis and treatment critical. A chest CT scan is often used to detect thymoma or other mediastinal abnormalities. In some cases, the CT scan showed enlarged thymus, indicating the presence of thymoma or thymic hyperplasia. Surgical removal of the thymoma, combined with thymectomy, is the standard treatment approach and can lead to significant improvement in MG symptoms and potentially lead to remission. This approach may also reduce the need for long-term prednisone treatment, which is commonly used to manage MG symptoms.

Thymic Hyperplasia and Myasthenia Gravis
What is Thymic Hyperplasia?
Thymic hyperplasia refers to the enlargement of the thymus gland, often with an increased number of lymphoid follicles (lymphofollicular hyperplasia). It is commonly seen in patients with Myasthenia Gravis, especially younger individuals. Unlike thymoma, thymic hyperplasia is not a tumor but represents an abnormal immune response. Many patients wonder, "Is thymic hyperplasia dangerous?" While it's not typically dangerous on its own, it can contribute to the severity of Myasthenia Gravis symptoms. It's important to note that thymic hyperplasia is not cancer, addressing the common question, "Is thymic hyperplasia cancer?"
Thymic Hyperplasia Symptoms and Diagnosis
Thymic hyperplasia symptoms are often indistinguishable from general Myasthenia Gravis symptoms. However, in some cases, an enlarged thymus may cause local effects such as chest discomfort or difficulty breathing. Diagnosis of thymic hyperplasia typically involves imaging studies, with thymic hyperplasia CT scans showing an enlarged thymus being a common finding. The severity of symptoms can be classified using the the Myasthenia Gravis Foundation of America (MGFA) classification, which helps in determining the appropriate treatment approach.
Treatment Implications
Thymic hyperplasia treatment often includes thymectomy, which can be beneficial for patients with this condition. Removing the enlarged thymus may help reduce the autoimmune attack on neuromuscular junctions, leading to improved symptoms and reduced medication needs, including corticosteroids like prednisone. In addition to thymectomy, other treatments for Myasthenia Gravis may include immunosuppressive treatment and plasma exchange therapy.
It's important to note that after thymectomy, some patients may experience thymic rebound or rebound thymic hyperplasia. This occurs when residual thymic tissue grows back, potentially causing a recurrence of symptoms. Residual thymic tissue symptoms can mimic the original Myasthenia Gravis symptoms, making regular follow-up and monitoring essential to detect and manage any post-thymectomy complications. Post-thymectomy improvement often takes months to years, and not all patients achieve remission – managing expectations is key.
In rare cases, thymoma or severe thymic hyperplasia can lead to superior vena cava syndrome, a condition where the superior vena cava becomes obstructed, causing various symptoms related to impaired blood flow.
In conclusion, understanding the complex relationship between the thymus and Myasthenia Gravis is crucial for effective management of this autoimmune disease. Whether dealing with thymoma, thymic hyperplasia, or considering thymectomy, patients should work closely with their healthcare providers to determine the best course of treatment for their individual case. It's also worth noting that Myasthenia Gravis can be associated with other autoimmune conditions, such as Graves' disease, highlighting the importance of comprehensive care and monitoring for patients with MG. The presence of anti-AChR antibodies and the potential benefits of thymectomy in reducing the need for medications like prednisone underscore the complexity of MG management and the importance of individualized treatment approaches.

have already shared their stories
Sources
- Thymectomy for Myasthenia Gravis: Analysis of the Controversies Regarding Technique and Results
Neurology, Vol 48, No suppl_5.
DOI: 10.1212/WNL.48.Suppl_5.52S . - The Role of Thymectomy in Myasthenia Gravis: A Programmatic Approach to Thymectomy and Perioperative Management of Myasthenia Gravis
Advances in Health and Disease, 2021.
DOI: 10.1016/j.athoracsur.2016.08.052 . - Thymectomy in Myasthenia Gravis: A Narrative Review
Saudi Journal of Medicine and Medical Sciences, 2022; 10(2): 97-104.
DOI: 10.4103/sjmms.sjmms_80_22 . - Randomized Trial of Thymectomy in Myasthenia Gravis
New England Journal of Medicine, 2016; 375:511-522.
DOI: 10.1056/NEJMoa1602489 . - The Impact of Thymectomy in Subgroups of Myasthenia Gravis Patients: A Single Center Longitudinal Observation
Journal of Thoracic Disease, 2023; 15(3): 123-130.
DOI: 10.21037/jtd-22-1591 .