Myasthenia Gravis: Understanding Receptors & Pathophysiology
.jpg)

have already shared their stories
Myasthenia Gravis (MG) is a condition that can feel like a mystery if you're not familiar with its inner workings. But don't worry, we're here to help you break it down. Imagine your muscles as a group of people trying to communicate, and Myasthenia Gravis disease as the static that disrupts their conversation. In this article, we'll explore how this static happens by diving into the pathophysiology of Myasthenia Gravis, focusing on receptors and mechanisms. We aim to make this complex condition more understandable, so you can better navigate the journey if you or a loved one is affected.
What is the Pathophysiology of Myasthenia Gravis?
Pathophysiology is a term that combines two concepts: "pathology" and "physiology."
- Pathology refers to the study of diseases, including their causes and effects on the body.
- Physiology is the study of how the body and its systems normally function.
So, pathophysiology looks at how diseases disrupt normal bodily functions. It helps us understand the changes that occur in the body when someone is sick, which can include changes at the cellular level, organ level, or in the entire system.
Overview of Myasthenia Gravis
Definition and Classification
The myasthenia gravis definition describes it as an autoimmune disorder that primarily affects the communication between nerves and muscles. This condition falls under a category of diseases where the immune system mistakenly attacks the body's own tissues, leading to muscle weakness. Generalized myasthenia gravis (GMG disease) is the most common form, affecting multiple muscle groups throughout the body.
Myasthenia Gravis as an Autoimmune Disease
As an autoimmune disease, Myasthenia Gravis represents a type of disease called "autoimmune neuromuscular disorder." This means that the body's defense system, including T cells and B cells, targets its own cells, specifically those at the neuromuscular junction, where nerves meet muscles. The myasthenia gravis hypersensitivity type is classified as Type II, involving antibody-mediated cytotoxicity.
Myasthenia Gravis Mechanism of Action
Role of Acetylcholine in Myasthenia Gravis
Acetylcholine is a chemical messenger that plays a crucial role in muscle contraction. In Myasthenia Gravis, the transmission of acetylcholine is interrupted, leading to the hallmark symptom of muscle weakness. Myasthenia gravis acetylcholine interactions are key to understanding the disease process.
Interaction at the Neuromuscular Junction
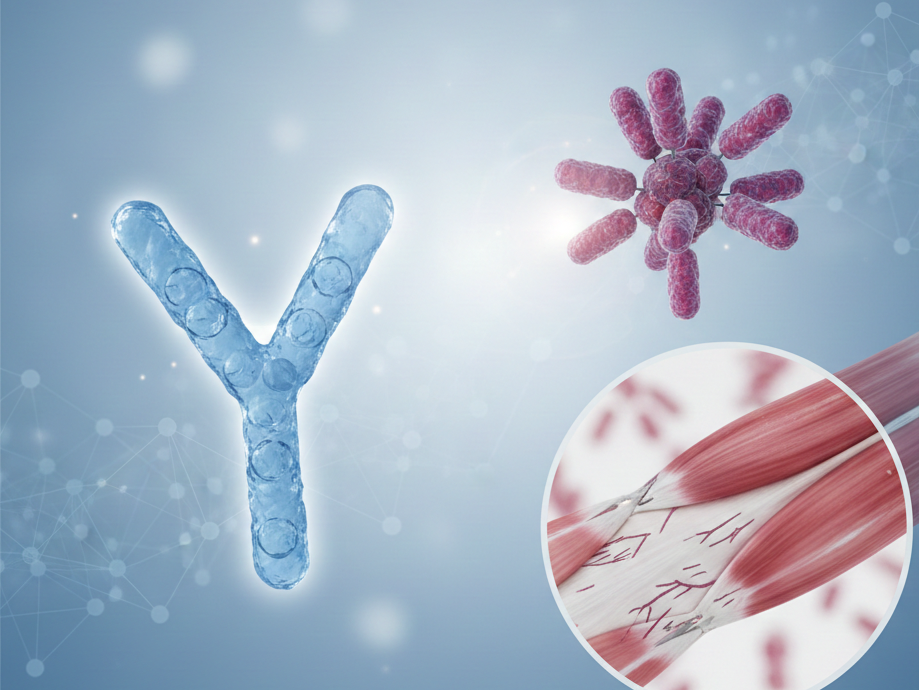
The neuromuscular junction is like a busy intersection where nerves and muscles communicate. In Myasthenia Gravis, this interaction is disrupted, as myasthenia gravis antibodies interfere with the signals that should tell muscles to contract. These antibodies target the nicotinic acetylcholine receptors on the postsynaptic membrane, preventing proper signal transmission.
How Do Receptors Contribute to Myasthenia Gravis?
Myasthenia Gravis Receptors and Antibodies
Acetylcholine Receptors and Their Function
Acetylcholine receptors are the communication points on muscle cells that receive signals from nerves. In Myasthenia Gravis, these receptors are blocked or destroyed by antibodies, hindering their function. In some cases, antibodies may target muscle-specific kinase (MuSK), another crucial protein at the neuromuscular junction.
Role of MG Antibodies in Myasthenia Gravis
MG antibodies act like uninvited guests that disrupt the party. They attack acetylcholine receptors, preventing nerve signals from reaching muscles, which causes the characteristic muscle weakness. The presence of these myasthenia gravis antibodies is a key factor in diagnosing the condition.
Impact on Neuromuscular Transmission
When receptors are compromised, neuromuscular transmission suffers. This breakdown means that muscles don't receive the messages they need to contract effectively, leading to the symptoms of Myasthenia Gravis.
Pathogenesis of Myasthenia Gravis
Immune System Involvement
Autoantibody Production
In the pathogenesis of Myasthenia Gravis, the immune system erroneously produces autoantibodies that target and damage acetylcholine receptors, disrupting normal muscle function. T cells play a crucial role in this process by helping B cells produce these harmful antibodies. The interaction between T cells and B cells involves various cytokines, which are signaling molecules that mediate immune responses.
Thymus Gland's Role
The thymus gland, part of the immune system, often plays a pivotal role in Myasthenia Gravis. It can become enlarged or develop a thymoma, contributing to the production of harmful antibodies. The presence of a thymoma is associated with a more severe form of the disease in some cases. Thymectomy, the surgical removal of the thymus gland, is sometimes recommended as a treatment option.
Presentation of Myasthenia Gravis
Common Symptoms and Signs
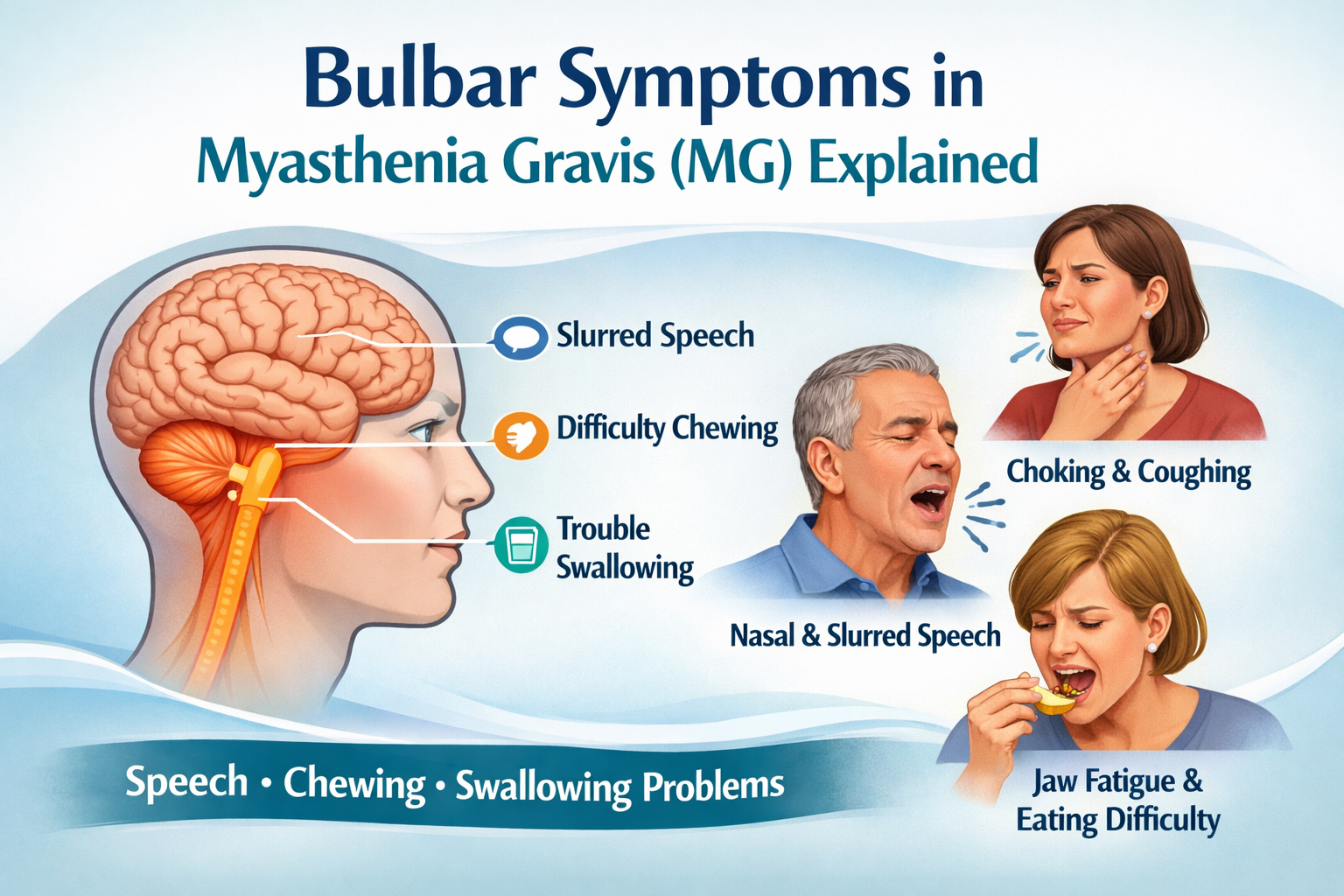
The presentation of Myasthenia Gravis often includes muscle weakness that worsens with activity and improves with rest. This can affect eye movement, facial expression, chewing, talking, and swallowing. In cases of mild myasthenia gravis, face muscles may be predominantly affected. Some patients may experience bulbar symptoms, which involve difficulties with speech and swallowing.
Diagnostic Criteria and Testing
Diagnosing Myasthenia Gravis typically involves clinical exams, antibody tests, and sometimes imaging of the thymus gland. Electromyography (EMG) tests may also be used to assess muscle response and detect fatigable muscle weakness characteristic of the condition.
Myasthenia Gravis Mechanisms Explored
Breakdown of Neuromuscular Junction Communication
Disruption of Signal Transmission
In Myasthenia Gravis, the disruption of signal transmission at the neuromuscular junction is akin to a phone line cut mid-call. This disruption prevents muscles from responding to nerve signals, affecting the synaptic vesicles that store and release acetylcholine.
Effect on Muscle Contraction
Without proper signaling, muscle contraction becomes inconsistent and weak, leading to the fatigue and skeletal muscle weakness that characterize Myasthenia Gravis.
Myasthenia Gravis and AP Psychology Definition
Psychological Implications and Considerations
Living with Myasthenia Gravis can also have psychological effects. The unpredictability of symptoms can lead to anxiety and stress, highlighting the importance of psychological support in management.
Myasthenia Gravis Causes and Epidemiology
Understanding the myasthenia gravis causes is crucial for developing effective treatments. While the exact trigger is unknown, genetic factors, including certain HLA associations, may play a role in susceptibility to the disease. Environmental factors and hormonal changes are also being studied as potential contributors.
Regarding myasthenia gravis epidemiology, recent studies have shed light on the condition's prevalence and incidence. The myasthenia gravis prevalence is estimated to be around 14-20 per 100,000 people, with the myasthenia gravis incidence rate at approximately 0.3-2.8 per 100,000 person-years. These myasthenia gravis statistics help researchers and healthcare providers better understand the disease's impact on populations.
Frequently Asked Questions
What are the early signs of Myasthenia Gravis?
Early signs often include drooping eyelids, double vision, and muscle weakness that improves with rest. These ocular symptoms are typically the first manifestation of the disease.
How is Myasthenia Gravis diagnosed?
Diagnosis involves clinical evaluations, blood tests for antibodies (including acetylcholine receptor antibodies and anti-MuSK antibodies), and sometimes imaging or EMG tests to assess muscle function.
Can Myasthenia Gravis be cured?
While there is no cure, treatments such as medications, lifestyle changes, and sometimes surgery can manage symptoms effectively. Thymectomy, the surgical removal of the thymus gland, can be beneficial for some patients, especially those with thymoma.
What are the treatment options for Myasthenia Gravis?
Treatment options include acetylcholinesterase inhibitors, immunosuppressive agents like prednisone, azathioprine, and mycophenolate mofetil. For more severe cases, rituximab or intravenous immune globulin may be used. Plasmapheresis, a procedure that removes harmful antibodies from the blood, is sometimes employed in crisis situations. Thymectomy is also considered in certain cases.
How does Myasthenia Gravis affect daily life?
The condition can impact daily activities, requiring adjustments to manage fatigue and muscle weakness, but with proper treatment, many individuals lead active lives. Understanding the disease's mechanisms, such as the role of voltage-gated calcium channels and complement activation, can help patients better manage their condition.
Understanding Myasthenia Gravis involves unraveling the complexities of receptors and immune mechanisms, but armed with knowledge, those affected can navigate this journey more confidently. Remember, you're not alone in this—support and resources are available to help you every step of the way. Ongoing myasthenia gravis research continues to improve our understanding of the disease's epidemiology, prevalence, and potential new treatments.
To further illustrate the complex mechanisms involved in Myasthenia Gravis, a myasthenia gravis diagram can be a helpful visual aid. These diagrams often depict the neuromuscular junction, showing how antibodies interfere with acetylcholine receptors and disrupt signal transmission.
Lastly, it's worth noting that myasthenia gravis demographics show that the condition can affect people of all ages and ethnicities. However, there are some patterns in its occurrence. For instance, it's more common in women under 40 and men over 60. Understanding these demographic trends can help in early detection and targeted research efforts.

have already shared their stories