Cholinergic Crisis Symptoms: Signs, Treatment & Antidote


have already shared their stories
Cholinergic Crisis Symptoms: Signs, Treatment & Antidote
Three million people worldwide suffer from organophosphate poisoning each year, and 300,000 of these cases turn fatal. These numbers explain why acetylcholine toxicity needs immediate medical intervention to prevent life-threatening complications.
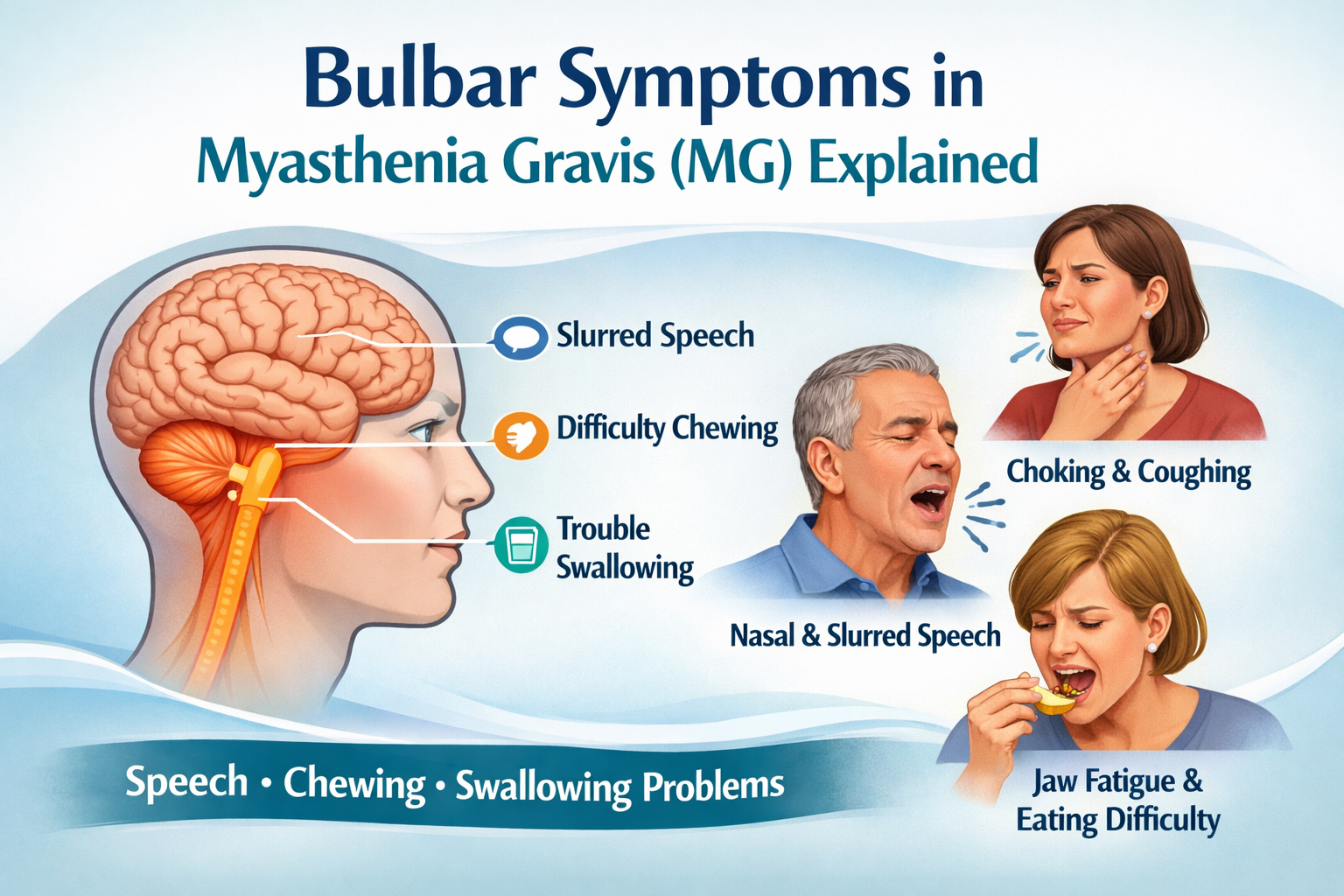
A cholinergic crisis occurs if acetylcholine levels become excessive in our bodies. Patients with myasthenia gravis face this dangerous condition due to medication overdose. Exposure to specific insecticides or nerve agents can also trigger this crisis. Patients experience multiple severe symptoms - excessive sweating, increased saliva production, muscle weakness, blurred vision and difficulty breathing.
Medical professionals need to spot the warning signs and life-threatening symptoms quickly. The right treatment at the right time saves lives. Mortality rates climb between 3% to 25% without proper medical care. Everything in this condition demands swift recognition and appropriate treatment to prevent fatal outcomes.
Early Warning Signs of High Acetylcholine Levels
Your body shows warning signs of acetylcholine toxicity before you realize you're in danger. Acetylcholine buildup in the body overstimulates receptors throughout your nervous system. This creates a cascade of unmistakable symptoms.
Excessive Sweating and Salivation: The First Red Flags
High acetylcholine levels often show up as excessive sweating (hyperhidrosis) at the time your body starts reacting. This happens because acetylcholine overstimulates cholinergic receptors on your eccrine sweat glands [1]. You might notice unusual amounts of sweat on your palms, soles, face, and underarms—areas packed with these glands.
Your salivary glands face the same overstimulation, which leads to increased saliva production. This excessive salivation, or "sialorrhea," fills your mouth with fluid and can feel uncomfortable.
Medical professionals use acronyms SLUDGE or DUMBELS to track these early muscarinic effects. The "S" represents salivation and "D" stands for diaphoresis (excessive sweating) [2].
Stomach Troubles: Nausea, Cramping, and Diarrhea
Your digestive system reacts faster as acetylcholine speeds up food movement through your tract. You might experience:
- Sudden nausea and vomiting
- Painful abdominal cramping
- Urgent, watery diarrhea
These symptoms appear because excess acetylcholine increases gastrointestinal motility, which makes your intestines contract more forcefully [3]. These digestive issues serve as significant warning signs that need attention.
Vision Changes and Teary Eyes
Changes in vision point to another early sign of cholinergic toxicity. Acetylcholine overload affects your eyes in several ways:
Your pupils constrict abnormally (miosis) and become unusually small even in dim lighting [4]. This pupil constriction makes it hard to focus.
Your lacrimal glands produce too many tears—called lacrimation—which leads to watery, blurry vision [3]. Someone reporting these vision changes along with other symptoms might have acetylcholine toxicity.
Feeling Short of Breath: The Time to Act
Breathing problems need immediate medical help since they can turn life-threatening faster. The first signs include:
- Chest tightness
- Wheezing
- Increased mucus production
Acetylcholine causes your bronchial tubes to constrict while stimulating mucus-producing glands in your airways [5]. These early breathing changes signal potential danger. This becomes especially important since breathing failure remains the main cause of death in acetylcholine toxicity cases [6].
Quick recognition of these warning signs could save lives. A cholinergic crisis can quickly turn from uncomfortable symptoms to breathing failure without proper medical help.
Life-Threatening Cholinergic Toxicity Symptoms
Untreated cholinergic toxicity can turn uncomfortable symptoms into life-threatening emergencies faster than you might expect. Medical professionals need to spot these warning signs quickly because they can mean the difference between life and death.
Respiratory Distress: When Breathing Becomes Difficult
Respiratory failure kills most patients in cholinergic crisis. Several things happen at once - airways tighten from bronchospasm, the lungs fill with excessive secretions (bronchorrhea), and breathing muscles get weaker. The diaphragm and muscles between the ribs can become completely paralyzed and stop breathing altogether. Research shows that respiratory failure can develop within hours after serious exposure [5].
Muscle Weakness and Fasciculations
Too much acetylcholine at nicotinic receptors creates specific muscle problems. You might notice the first sign - muscle twitching or fasciculations that look like small contractions under the skin. These symptoms can lead to severe muscle weakness. This weakness can become so bad that muscles stop working completely, a condition called flaccid paralysis [4]. The breathing muscles and diaphragm often suffer this effect, which makes it even harder to breathe [2].
Heart Rate Changes and Blood Pressure Problems
Your cardiovascular system faces serious risks too. Your heart might beat too slowly (bradycardia) or sometimes surprisingly fast. Blood pressure becomes unpredictable - it might drop very low or spike dangerously high [5]. People who already have heart problems face the biggest risks. The most severe cases can develop irregular heartbeats that may lead to cardiovascular collapse and death [2].
Mental Status Changes: Confusion to Seizures
The effects on your brain can range from mild to devastating. You might notice confusion and headaches first. The situation can get worse with agitation, slurred speech, and sleepiness [5]. The most serious cases involve seizures that can turn into status epilepticus - where seizures don't stop [7]. Studies show that seizures happen more often in children (25%) than adults (2.5%) who are exposed to organophosphates [8]. These seizures can put someone in a coma and cause major brain damage if left untreated [8].
Emergency Treatment for Acetylcholine Toxicity
Time matters most when treating acetylcholine toxicity. A proper emergency response can save lives, whether the cause stems from pesticide exposure, medication overdose, or nerve agents.
First Aid and When to Emergency
You should call emergency services right away if you notice multiple cholinergic symptoms like excessive secretions, breathing problems, muscle twitching, or confusion. These vital steps can help while waiting for emergency responders:
- Remove the exposure source - Take off contaminated clothing with care and wash exposed skin using soap and water at least three times. This prevents further absorption and protects others from cross-contamination.
- Ensure ABC (Airway, Breathing, Circulation) - Keep the person's airway open. Turn them to their side if unconscious to stop secretions from being aspirated.
- Do not induce vomiting or give anything by mouth to someone who's unconscious.
The suspected toxin container or medication should go to the hospital with the patient since identifying the specific agent helps determine the right treatment.
Hospital Interventions: What to Expect
The medical team focuses on life-saving measures once you reach the emergency department:
Initial Stabilization: The medical team will secure the airway if needed, which might require intubation if breathing becomes severely compromised. Doctors consider intubation with copious secretions, Glasgow Coma Score below 8, hemodynamic instability, or severe respiratory muscle weakness.
Antidote Administration: Treatment's life-blood consists of two crucial medications:
- Atropine: This counteracts muscarinic effects (excessive secretions, bronchospasm) but doesn't help muscle weakness. Doctors continue dosing until "atropinization" appears—dry skin, increased heart rate, and dilated pupils.
- Pralidoxime (2-PAM): This acts as a "molecular crowbar" to separate organophosphates from acetylcholinesterase and restores normal enzyme function, especially for muscle strength.
Supportive Care: The treatment includes intravenous fluids, cardiac monitoring, seizure management with benzodiazepines, and intensive care unit admission for severe cases.
Most patients recover with quick, appropriate treatment, though they might need respiratory support from hours to days based on exposure severity.
Cholinergic Crisis Antidotes and Medications
Two powerful antidotes are the foundations of cholinergic crisis treatment that defend against acetylcholine toxicity. Learning about these medications helps explain their vital role in emergency care.
How Atropine Works to Counter Cholinergic Effects
Atropine blocks acetylcholine from binding to muscarinic receptors throughout the body as a competitive antagonist [9]. This blockade stops excess acetylcholine from triggering dangerous symptoms like excessive secretions and bronchospasm.
Doctors give atropine until they see signs of "atropinization":
- Dry mouth and skin
- Dilated pupils (mydriasis)
- Increased heart rate (tachycardia) [4]
Adult patients receive original doses of 2-5 mg intravenously, with more doses every 5-10 minutes until breathing improves [6]. Severe poisoning cases might need surprisingly high amounts of atropine that can exceed 100 mg [10].
Note that atropine works only on muscarinic receptors and doesn't help with muscle weakness or paralysis from nicotinic effects [11].
Pralidoxime (2-PAM) for Organophosphate Poisoning
Pralidoxime (2-PAM) tackles what atropine can't—the nicotinic effects of acetylcholine toxicity. It works like a "molecular crowbar" that pulls organophosphates away from the acetylcholinesterase enzyme, which lets normal acetylcholine breakdown start again [4].
Standard pralidoxime treatment uses 1-2 grams intravenously over 15-30 minutes and continues with an infusion of 8 mg/kg/hour [12]. Timing is critical with pralidoxime because the organophosphate-enzyme bond becomes permanent ("aging") and makes treatment useless [4].
Research shows mixed results about pralidoxime's benefits, and some studies question whether it works better than atropine alone [13].
Supportive Treatments and Breathing Support
Supporting vital functions remains vital alongside specific antidotes. About 20% of hospitalized patients need mechanical ventilation [14], and respiratory failure leads to most deaths in cholinergic poisoning [15].
Benzodiazepines control seizures effectively—doctors prefer diazepam over anti-epileptic drugs [5].
Doctors must never use succinylcholine during intubation because acetylcholinesterase inhibition makes its paralytic effects last too long [5].
The right combination of antidotes and supportive care helps more patients survive. Mortality stays around 2% in mild cases but rises to 15% when patients need mechanical ventilation [14].
Conclusion
Quick recognition and understanding of cholinergic crisis can save lives. This piece explores how this condition develops from early warning signs like excessive sweating and vision changes into complications that can affect breathing and heart function.
Here are the key points to remember:
- Early symptoms like SLUDGE signs (sweating, excessive saliva) are vital warning signals
- Breathing problems pose the most dangerous threat and need immediate medical care
- Treatment combines specific antidotes (atropine and pralidoxime) with supportive care
- Quick medical help improves survival rates by a lot
Better recognition and standardized emergency protocols help medical teams treat most cholinergic crisis cases successfully now. This condition responds well to proper treatment, especially when caught early. Recognizing these warning signs and taking swift action can mean the difference between life and death.
The symptoms need extra attention if you or someone you know takes medications for myasthenia gravis or works with organophosphate compounds. Proper medical care and fast action give you the best chance to recover fully from this serious but treatable condition.
FAQs
Q1. What are the primary antidotes used to treat a cholinergic crisis? The two main antidotes for cholinergic crisis are atropine and pralidoxime (2-PAM). Atropine counteracts muscarinic effects like excessive secretions, while pralidoxime helps restore normal enzyme function, particularly for muscle strength.
Q2. How quickly should treatment be administered in a cholinergic crisis? Treatment should be administered as quickly as possible. Cholinergic crisis can escalate rapidly, and prompt medical intervention significantly improves survival rates. Call emergency services immediately if you observe multiple cholinergic symptoms.
Q3. What are the early warning signs of acetylcholine toxicity? Early warning signs include excessive sweating, increased salivation, stomach troubles (nausea, cramping, diarrhea), vision changes, teary eyes, and feeling short of breath. These symptoms are often remembered using the acronym SLUDGE.
Q4. Can cholinergic crisis be fatal if left untreated? Yes, cholinergic crisis can be fatal if left untreated. Respiratory failure is the primary cause of death in these cases. Without proper intervention, symptoms can rapidly progress from uncomfortable to life-threatening.
Q5. What supportive treatments are used alongside antidotes in cholinergic crisis? Supportive treatments include mechanical ventilation for respiratory support, intravenous fluids, cardiac monitoring, and seizure management with benzodiazepines. Severe cases may require admission to the intensive care unit for comprehensive management.

have already shared their stories





.png)
.png)