Myasthenia Gravis: Understanding Dysphagia, Treatments & Solutions
.avif)

have already shared their stories
Living with myasthenia gravis (MG), a complex neuromuscular disease, can be challenging, especially when it affects your ability to swallow. Dysphagia, or difficulty swallowing, is a common issue for those with this condition. But don't worry—there are effective treatments and strategies to help you manage these symptoms and improve your quality of life. In this guide, we'll explore what causes swallowing difficulties and discuss treatment options, lifestyle adjustments, and more.
What Causes Difficulty Swallowing in Myasthenia Gravis?
Understanding Myasthenia Gravis and Its Impact on Swallowing
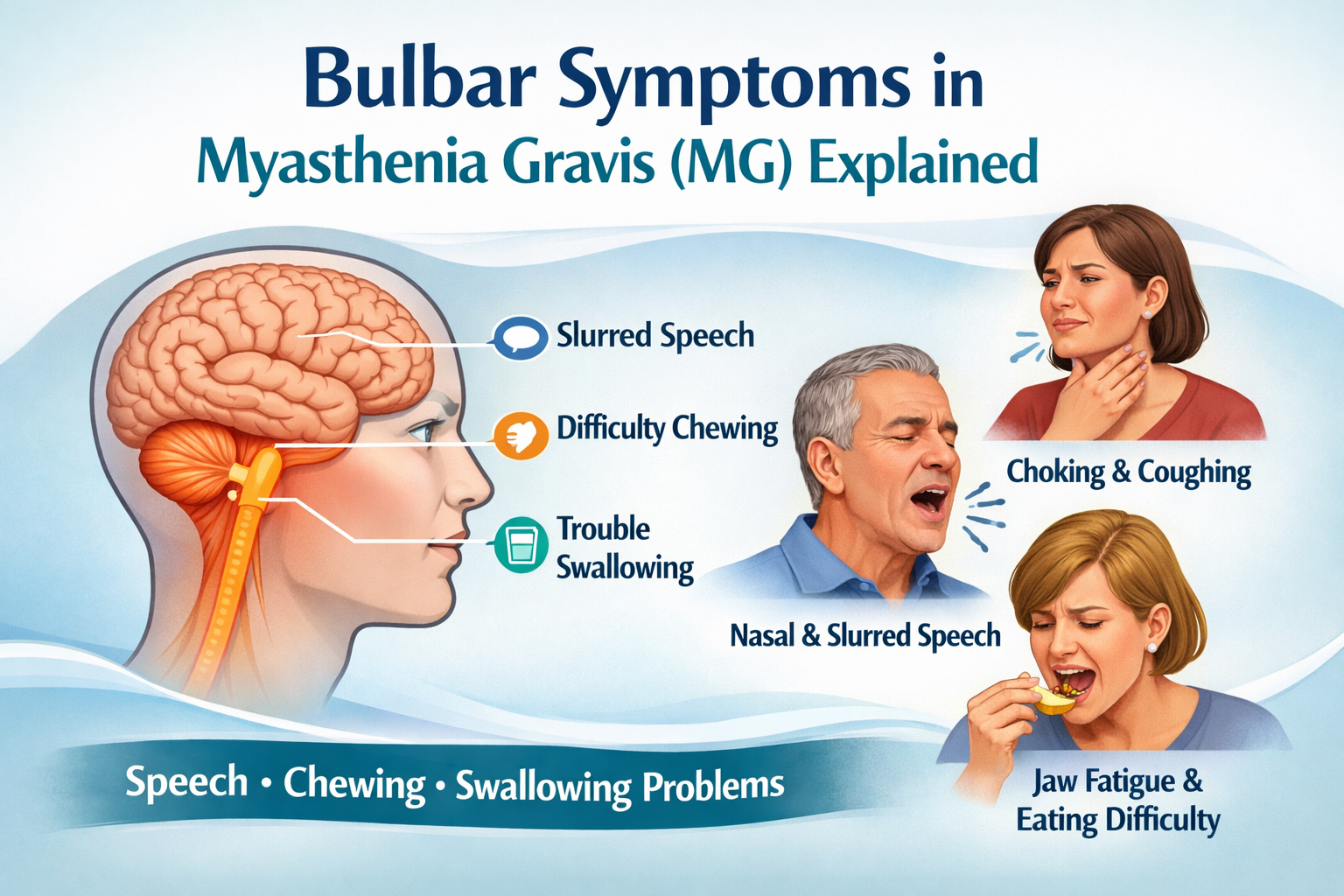
Myasthenia gravis is an autoimmune disorder that affects acetylcholine receptors, weakening the skeletal muscles responsible for voluntary movements. When the oropharyngeal muscles in the throat and esophagus are affected, it can lead to swallowing problems. This difficulty in swallowing, known as dysphagia (sometimes misspelled as dysphasia, which is a completely different symptom, referring to speech difficulties), can make eating and drinking a daily struggle and may contribute to communication challenges.
How Myasthenia Gravis Leads to Dysphagia
The primary cause of dysphagia in myasthenia gravis patients is muscle weakness and fatigability. The muscles involved in swallowing can become fatigued, making it hard to move food and liquids from the mouth to the stomach. This can result in coughing, choking, or even aspiration, where food enters the lungs, potentially leading to pneumonia. The condition can also impact the myasthenia gravis tongue function, further complicating the swallowing process.
What Are the Treatment Options for Myasthenia Gravis Dysphagia?
Medications to Manage Dysphagia Symptoms
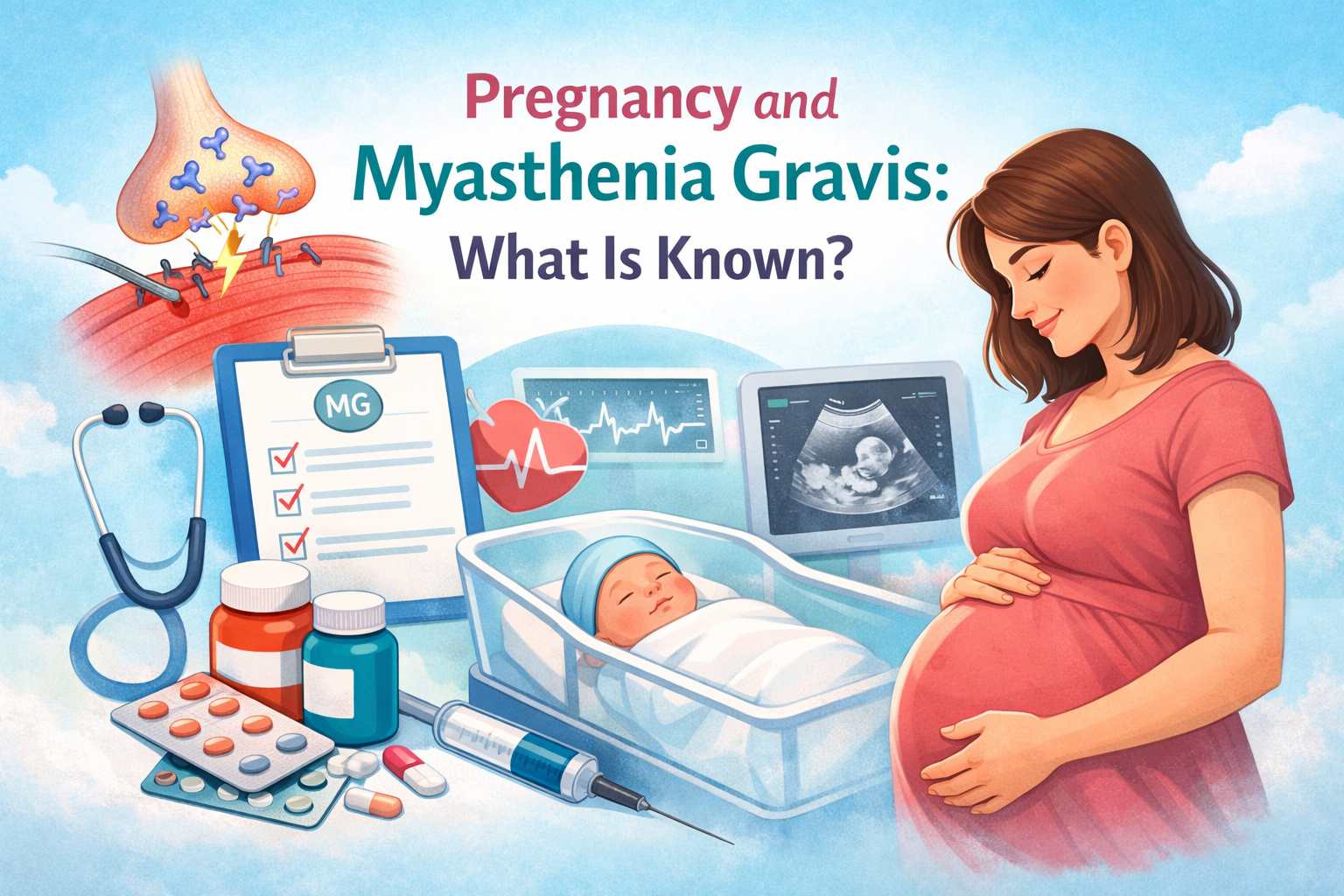
Managing dysphagia in myasthenia gravis often starts with medications that help improve muscle strength and reduce fatigue. Anticholinesterase agents like pyridostigmine work by enhancing communication between nerves and muscles, making it easier to swallow. For those with more severe or treatment-resistant MG, newer therapies such as monoclonal antibodies have expanded the options. Eculizumab, a complement inhibitor, and efgartigimod, which targets the neonatal Fc receptor, have both been approved for generalized MG and have shown effectiveness in easing symptoms—including swallowing difficulties. Because each case is different, it’s essential to work closely with your healthcare provider to find the right combination of treatments and dosages. This not only helps manage daily symptoms but also reduces the risk of serious complications like a myasthenic crisis.
The Role of Speech Therapy in Treating Swallowing Problems
Speech therapy, conducted by a qualified speech-language pathologist, is a valuable component of managing dysphagia. These professionals are trained to help patients improve their swallowing function through targeted exercises and techniques.
Speech Therapy Techniques
Speech therapists use various techniques to strengthen the muscles involved in swallowing. These may include exercises to improve tongue mobility, increase throat muscle strength, and enhance coordination. Myasthenia gravis speech therapy often focuses on addressing both dysphagia and dysarthria, a speech disorder that can accompany the condition. The myasthenia gravis dysarthria type can vary, but it typically affects the clarity and strength of speech.
Myasthenia Gravis Swallowing Exercises
Swallowing exercises are designed to improve the function and coordination of the swallowing muscles. Simple exercises, such as swallowing multiple times in a row or practicing with different textures of food, can be effective. Your therapist will tailor a program to your specific needs and abilities, which may include oral motor exercises for dysphagia. PDF resources are often available to guide patients through these exercises at home.
Oral Dysphagia Treatment
Oral dysphagia treatment often involves a combination of strengthening exercises, compensatory techniques, and postural techniques. These methods aim to make swallowing safer by improving the pharyngeal phase of swallowing, enhancing epiglottic inversion, and promoting proper laryngeal elevation; these are the movements that help keep food from going into the airway. Speech therapists establish specific dysphagia goals for speech therapy to track progress and adjust treatment plans as needed. These goals are crucial in ensuring that the therapy is effective and tailored to each patient's unique challenges.
Lifestyle and Dietary Adjustments for Swallowing Difficulties
Dietary Changes to Ease Swallowing
Adjusting your diet can make swallowing easier and safer. Consider softer foods, such as purees and soups, that require less effort to swallow. Staying hydrated is also crucial, so aim for regular sips of water throughout the day. For those wondering how to lose weight with myasthenia gravis, working with a nutritionist can help balance dietary needs with swallowing capabilities. A dietitian can help tailor a nutrition plan that accommodates swallowing difficulties while ensuring adequate caloric and nutrient intake. Their expertise is vital not only in selecting appropriate food textures but also in preventing malnutrition—a common risk for patients with dysphagia.
Tips for Safe Eating and Drinking
Eating smaller, more frequent meals can help manage swallowing difficulties. Take your time, chew thoroughly, and avoid talking while eating to minimize the risk of choking. Sitting upright during meals can also aid in safe swallowing. In some cases, augmentative alternative communication methods may be helpful during mealtimes to reduce the risk of aspiration. Additionally, practicing good vocal hygiene can help maintain overall oral health and reduce strain on the muscles involved in swallowing and speaking.
The Importance of Monitoring and Ongoing Care
Working with Healthcare Professionals
Regular check-ins with your healthcare team are vital for managing MG and dysphagia. They can help monitor your progress and make necessary adjustments to your treatment plan. This may include periodic swallowing evaluations and videofluoroscopy studies to assess swallowing function. Videofluoroscopy is a dynamic imaging technique that allows healthcare providers to visualize the swallowing process in real-time, helping to identify specific areas of difficulty.
Keeping Track of Symptoms and Progress
Maintaining a journal to track your symptoms, including bulbar symptoms and vocal fatigue, can be beneficial. This information can help your healthcare provider tailor treatments to your needs and adjust dysphagia management strategies as necessary. Regular videofluoroscopy and swallowing evaluation sessions can provide objective data on your progress over time.
Frequently Asked Questions
What are the first signs of dysphagia in myasthenia gravis?
Early signs of dysphagia may include frequent coughing or choking during meals, a sensation of food sticking in the throat, or unexpected weight loss due to difficulty eating. Patients may also experience dysarthria, a type of speech difficulty associated with the condition. Dysarthria can manifest as slurred speech or difficulty articulating certain sounds.
How effective is speech therapy for swallowing problems in myasthenia gravis?
Speech therapy can be highly effective in managing swallowing issues, as it focuses on strengthening the muscles and improving coordination, leading to better swallowing function. Speech-language pathologists set specific dysphagia goals for speech therapy to ensure treatment efficacy and monitor patient progress. These goals are tailored to each individual's needs and adjusted as necessary throughout the therapy process.
Are there any specific swallowing exercises recommended for myasthenia gravis patients?
Yes, exercises such as the Mendelsohn maneuver, effortful swallows, and tongue-hold swallows are often recommended. Your speech therapist can provide personalized exercises based on your condition and may include specific myasthenia gravis teaching materials, such as oral motor exercises for dysphagia PDF guides.
Can dietary changes significantly improve swallowing difficulties?
Absolutely. Dietary changes can reduce the effort required for swallowing and lower the risk of choking, making mealtime safer and more comfortable. Environmental adaptations may also be recommended to support safe eating habits and address communication challenges associated with mealtimes.
How can I find a specialist for myasthenia gravis dysphagia treatment?
Start by asking your primary care doctor for a referral to a speech-language pathologist or a neurologist who specializes in myasthenia gravis. You can also reach out to local support groups for recommendations on specialists experienced in treating neuromuscular diseases and managing communication challenges related to dysarthria.
Remember, managing myasthenia gravis and its associated swallowing difficulties is a journey. With the right combination of medical treatment, therapy, and lifestyle adjustments, many patients find significant improvement in their symptoms and quality of life.

have already shared their stories